 |
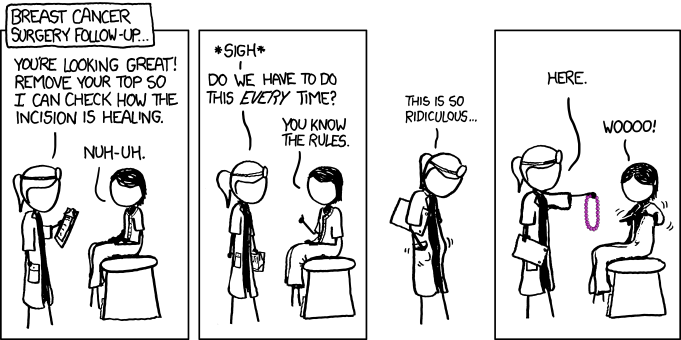
| Diamonds would work too (Click to enlarge) |
Blogging my life with breast cancer, from suspicion to diagnosis to treatment. Now livin' the Stage IV Lifestyle! Terminal Cancer can be funny. Just not for very long.
Pages
▼
Friday, December 30, 2011
Thursday, December 29, 2011
***Final Report***
Have you ever noticed that radiologists can't write? I have read enough radiology reports in my life to know the difference between writing medically and plain old poor writing. Radiologists either have so many reports to do that in their haste they make grammatical and word choice errors - or they purely can't write.
I'd love to see a Christmas newsletter from one of these guys:
"Insofar as Christmas went, it was a freely-flowing event, which is probably due to the unremarkable nature of the people incurred. The weather was of minimal hazy density, and winter structures intact. Facial rictus may represent Christmas cheer."
Anyway, I got excellent news on my latest scan, and I'm still kind of in shock as I no longer expect good news and me to be in the same place.
My bad.
I wanted to have my results sent to my oncologist, since the Infectious Disease Specialist, who ordered my scan "STAT," promptly went on vacation and was not available to go over it with me. I had my Wednesday herceptin/doctor appointment yesterday, so with the help of my Case Manager, I got the paperwork sent to my "Onc" so he could go over it with me. HIPPA does not make things easy.
I sat down with my doctor who read it in the exam room and went over the salient points with me. He said I had some thickening in the wall of the colon but it is resolving well. I'm healing. I asked him if the thickening was causing the pain and he said "probably." He said that there is fluid in my right lung but that he's not worried about it. He thinks it may be leftover from the surgery, and it doesn't appear that cancer has gotten into my lungs, which would have alarmed me had I even considered it. He did say they only imaged the bottom of the lungs, but I told him I'm not having any symptoms and didn't even know there was fluid in my lungs. I know breast cancer spreads to lungs but I don't think it has - he doesn't either; he said it would have grown big by now.
I did say I can't cough because my colon hurts too much. He didn't respond - maybe it's not that kind of fluid.
The most exciting thing he said - and I wish I could remember his exact wording - was, "There are no signs of cancer in your liver." OR, he said, "There are no new signs of cancer in your liver" OR "Your liver looks good, no cancer." I was very excited by my initial interpretation (no cancer period) and said that was a great relief since it had been so long since I'd been able to do chemo. I'd have expected to have a liver full of cancer again, and was thrilled I didn't. He didn't dissuade me from my excitement so I assume my interpretation is correct. Maybe they cured me after all, even with this setback.
His main concern is my weight. He said at my appointment right before Thanksgiving I weighed 105, and now I'm 90. A significant weight loss, yes. He was concerned that if something "put me down" that I had no fat at all as protection, and I would get bedsores.
I thought that was a funny, if a typical, thing to worry about. People in the medical profession seem unduly concerned about bedsores. When I was in the hospital I had to have regular bedsore checks; it was mentioned a lot by everybody, and they kept bringing me a foul-smelling creme that would help prevent them. (Really, why can't they get a contract with Bath and Body Shop or Origins or some company that makes a less industrial smelling creme - then maybe we'd use their bed sore preventatives). I guess they are overly worried because it's something they get sued over, but maybe it's more dangerous than I would have expected.
Having no fear of bedsores at my age, but having a great fear of c-diff, I told the doctor that we'd have to hope nothing would put me down for a while. I told him I realized I was too thin, and I wanted to gain weight but eating makes me nauseous. He suggested I try a compezine before mealtime. If you look at what you are allowed to eat with colitis, it is exactly the opposite of the way I normally eat. I am a fruit, veggie, high fiber girl, and those are not things I can eat right now without causing great intestinal pain. So, not only do I have to eat carefully, I have to change my entire diet. It does make me not want to eat too but I'll have to try harder.
I asked when I could start chemo again, and he said I'd know when I felt healthy enough. He made an appointment for a month from now, so my goal is to somehow recover by then. I need to gain at least five pounds, have this pain gone, not be nauseated when I eat and regain my physical strength. (ie., be able to go to Macy's and open their glass door.)
Anyway, out of all the myriad things that could go wrong with me, and that have gone wrong with me, being told I'm ten pounds underweight is about the best news I could have possibly heard.
I'll definitely be celebrating the New Year, even if it's with plain mashed potatoes and water.
So, here is the medical report. I will mark in bold a confusing part.
FINDINGS ABDOMEN: There is a new small freely flowing left basal pleural effusion. There is minimal hazy density in the posterior aspect of the right lung base which is thought to be atelectasis rather than pneumonia. The lung bases are otherwise clear as insofar visualized. There are no definite pulmonary or pleural-based nodules or masses seen. What is seen of the heart is unremarkable. (Edit: I would disagree with that statement; I have quite a remarkable heart.) What appear to be right breast prosthesis and left breast implant are grossly intact appearing. (Edit: I would agree with the "grossly intact" statement; had he said grotesquely it might have been more accurate.) What little is seen of breast tissues is unremarkable. (Again, I agree.)
Liver and spleen are homogeneous without focal mass or enlargement. (No mass! Great... until you read the end, where it gets confusing.) The patient has had resection of much of the left lobe of the liver apparently for neoplastic lesions in the interval between the current and August 2011 scans, and there is a linear band of low attenuation some 1.3 cm in diameter extending out obliquely through the anterior segment of the right lobe of the liver which is probably had treatment of a lesion in the central right lobe of the liver. (Edit: this is where they did the ablation.) When we look back at the scan of 08/08/11, there was a low attenuation roughly 2 cm in diameter area in the mid right lobe of the liver which has decreased to 1.5 cm. There are no new liver masses or nodules identified. (Not knowing exactly what that meant, confused by the term "new" I decided that the area that was burned away in the ablation is now healing and is now 1.5 (or 1.3) cms. I found this sentence online that backs me up: "On CT scans, complete ablation is seen as a low-attenuation area devoid of enhancement or nodules, as described earlier.)
If you have a better idea, or you are a radiologist, let me know.
Gallbladder, pancreas, adrenals, and kidneys are grossly unremarkable. The same is true of GI, vascular, and skeletal structures in the abdomen except that there is a question of colitis with wall thickening seen in all of the loops of the colon. Perhaps the patient is recovering from pseudomembraneous colitis. I do not see any ascites or lymphadenopathy in the pelvis.
PELVIS: Ureters and bladder, and uterus and adnexa (I have a body part called an adnexa?) are unremarkable appearing as are vascular and skeletal structures. GI structures are notable for mild wall thickening throughout the colon which as discussed above might represent resolving pseudomembranous colitis. There is no abscess or free intraperitoneal air.
In the interval between current and most recent comparison study, the patient has developed a small freely flowing right pleural effusion (didn't it say left in the first sentence?), apparent mild right lower lobe atelectasis, has apparently had treatment of central right liver nodule that has decreased in size from 2 cm to 1.5 cms (wait - it's a nodule now??? or I had treatment for a nodule and the space is 1.5 cms......) and has had resection of at least some of the left lobe of the liver. There is no new metastatic breast cancer demonstrated in the abdomen or pelvis.
Mild pancolitis may represent resolving pseudomenbraneous colitis. Clinical correlation recommended.
So, it appears to bealmost great news, except for the mild ambiguity on the report about the area in my right lobe, no doubt caused by poor writing skills, and hopefully not poor interpretation skills on my end. Until otherwise notified, I am choosing to believe there is no cancer and concentrate on healing my colitis. Considering how I feel, the fact that it is healing is fantastic news; I fully expected to be told there was an abscess considering how much lower right quadrant pain I still have. I guess it just takes time, and as we all know by now, patience is not my strong suit.
In any event.......
Happy Almost New Year! Looks like you might have me around for 2012 after all!
I'd love to see a Christmas newsletter from one of these guys:
"Insofar as Christmas went, it was a freely-flowing event, which is probably due to the unremarkable nature of the people incurred. The weather was of minimal hazy density, and winter structures intact. Facial rictus may represent Christmas cheer."
Anyway, I got excellent news on my latest scan, and I'm still kind of in shock as I no longer expect good news and me to be in the same place.
My bad.
I wanted to have my results sent to my oncologist, since the Infectious Disease Specialist, who ordered my scan "STAT," promptly went on vacation and was not available to go over it with me. I had my Wednesday herceptin/doctor appointment yesterday, so with the help of my Case Manager, I got the paperwork sent to my "Onc" so he could go over it with me. HIPPA does not make things easy.
I sat down with my doctor who read it in the exam room and went over the salient points with me. He said I had some thickening in the wall of the colon but it is resolving well. I'm healing. I asked him if the thickening was causing the pain and he said "probably." He said that there is fluid in my right lung but that he's not worried about it. He thinks it may be leftover from the surgery, and it doesn't appear that cancer has gotten into my lungs, which would have alarmed me had I even considered it. He did say they only imaged the bottom of the lungs, but I told him I'm not having any symptoms and didn't even know there was fluid in my lungs. I know breast cancer spreads to lungs but I don't think it has - he doesn't either; he said it would have grown big by now.
I did say I can't cough because my colon hurts too much. He didn't respond - maybe it's not that kind of fluid.
The most exciting thing he said - and I wish I could remember his exact wording - was, "There are no signs of cancer in your liver." OR, he said, "There are no new signs of cancer in your liver" OR "Your liver looks good, no cancer." I was very excited by my initial interpretation (no cancer period) and said that was a great relief since it had been so long since I'd been able to do chemo. I'd have expected to have a liver full of cancer again, and was thrilled I didn't. He didn't dissuade me from my excitement so I assume my interpretation is correct. Maybe they cured me after all, even with this setback.
His main concern is my weight. He said at my appointment right before Thanksgiving I weighed 105, and now I'm 90. A significant weight loss, yes. He was concerned that if something "put me down" that I had no fat at all as protection, and I would get bedsores.
I thought that was a funny, if a typical, thing to worry about. People in the medical profession seem unduly concerned about bedsores. When I was in the hospital I had to have regular bedsore checks; it was mentioned a lot by everybody, and they kept bringing me a foul-smelling creme that would help prevent them. (Really, why can't they get a contract with Bath and Body Shop or Origins or some company that makes a less industrial smelling creme - then maybe we'd use their bed sore preventatives). I guess they are overly worried because it's something they get sued over, but maybe it's more dangerous than I would have expected.
Having no fear of bedsores at my age, but having a great fear of c-diff, I told the doctor that we'd have to hope nothing would put me down for a while. I told him I realized I was too thin, and I wanted to gain weight but eating makes me nauseous. He suggested I try a compezine before mealtime. If you look at what you are allowed to eat with colitis, it is exactly the opposite of the way I normally eat. I am a fruit, veggie, high fiber girl, and those are not things I can eat right now without causing great intestinal pain. So, not only do I have to eat carefully, I have to change my entire diet. It does make me not want to eat too but I'll have to try harder.
I asked when I could start chemo again, and he said I'd know when I felt healthy enough. He made an appointment for a month from now, so my goal is to somehow recover by then. I need to gain at least five pounds, have this pain gone, not be nauseated when I eat and regain my physical strength. (ie., be able to go to Macy's and open their glass door.)
Anyway, out of all the myriad things that could go wrong with me, and that have gone wrong with me, being told I'm ten pounds underweight is about the best news I could have possibly heard.
I'll definitely be celebrating the New Year, even if it's with plain mashed potatoes and water.
So, here is the medical report. I will mark in bold a confusing part.
FINDINGS ABDOMEN: There is a new small freely flowing left basal pleural effusion. There is minimal hazy density in the posterior aspect of the right lung base which is thought to be atelectasis rather than pneumonia. The lung bases are otherwise clear as insofar visualized. There are no definite pulmonary or pleural-based nodules or masses seen. What is seen of the heart is unremarkable. (Edit: I would disagree with that statement; I have quite a remarkable heart.) What appear to be right breast prosthesis and left breast implant are grossly intact appearing. (Edit: I would agree with the "grossly intact" statement; had he said grotesquely it might have been more accurate.) What little is seen of breast tissues is unremarkable. (Again, I agree.)
Liver and spleen are homogeneous without focal mass or enlargement. (No mass! Great... until you read the end, where it gets confusing.) The patient has had resection of much of the left lobe of the liver apparently for neoplastic lesions in the interval between the current and August 2011 scans, and there is a linear band of low attenuation some 1.3 cm in diameter extending out obliquely through the anterior segment of the right lobe of the liver which is probably had treatment of a lesion in the central right lobe of the liver. (Edit: this is where they did the ablation.) When we look back at the scan of 08/08/11, there was a low attenuation roughly 2 cm in diameter area in the mid right lobe of the liver which has decreased to 1.5 cm. There are no new liver masses or nodules identified. (Not knowing exactly what that meant, confused by the term "new" I decided that the area that was burned away in the ablation is now healing and is now 1.5 (or 1.3) cms. I found this sentence online that backs me up: "On CT scans, complete ablation is seen as a low-attenuation area devoid of enhancement or nodules, as described earlier.)
If you have a better idea, or you are a radiologist, let me know.
Gallbladder, pancreas, adrenals, and kidneys are grossly unremarkable. The same is true of GI, vascular, and skeletal structures in the abdomen except that there is a question of colitis with wall thickening seen in all of the loops of the colon. Perhaps the patient is recovering from pseudomembraneous colitis. I do not see any ascites or lymphadenopathy in the pelvis.
PELVIS: Ureters and bladder, and uterus and adnexa (I have a body part called an adnexa?) are unremarkable appearing as are vascular and skeletal structures. GI structures are notable for mild wall thickening throughout the colon which as discussed above might represent resolving pseudomembranous colitis. There is no abscess or free intraperitoneal air.
In the interval between current and most recent comparison study, the patient has developed a small freely flowing right pleural effusion (didn't it say left in the first sentence?), apparent mild right lower lobe atelectasis, has apparently had treatment of central right liver nodule that has decreased in size from 2 cm to 1.5 cms (wait - it's a nodule now??? or I had treatment for a nodule and the space is 1.5 cms......) and has had resection of at least some of the left lobe of the liver. There is no new metastatic breast cancer demonstrated in the abdomen or pelvis.
Mild pancolitis may represent resolving pseudomenbraneous colitis. Clinical correlation recommended.
So, it appears to be
In any event.......
Happy Almost New Year! Looks like you might have me around for 2012 after all!
Saturday, December 24, 2011
Merry Christmas 2011
STAT meant stat, and I had my CAT scan yesterday. They were not done with me until after 5:00 pm, so I don't expect to hear from a doctor until Monday after the holiday. I'd like to think this pain is just a part of a long healing process - - - but I don't really think that's true.
But, the good news is I am going to have the quiet Christmas I dreamed of a couple of weeks ago. I'm not exactly healthy, but managed my Christmas shopping - thanks to Amazon Prime. Everybody gets something from me, and the gifts are wrapped too! While I can't stand up long enough to cook an elaborate meal, we can get a Honeybaked ham and side dishes. Mostly, I will be able to see my children and my husband and have a nice time with them. We'll open gifts, than play board games, listen to Christmas music and maybe drink hot cider and eat Christmas cookies. What could be better?!
People have also been very good to me this year, and I have more thanks to give out than I can possibly manage.
May you and yours have a very Merry Christmas - STAT!
But, the good news is I am going to have the quiet Christmas I dreamed of a couple of weeks ago. I'm not exactly healthy, but managed my Christmas shopping - thanks to Amazon Prime. Everybody gets something from me, and the gifts are wrapped too! While I can't stand up long enough to cook an elaborate meal, we can get a Honeybaked ham and side dishes. Mostly, I will be able to see my children and my husband and have a nice time with them. We'll open gifts, than play board games, listen to Christmas music and maybe drink hot cider and eat Christmas cookies. What could be better?!
People have also been very good to me this year, and I have more thanks to give out than I can possibly manage.
May you and yours have a very Merry Christmas - STAT!
Thursday, December 22, 2011
It's not how sick you are...it's who you know....
I have been trying to get an appointment with an infectious disease specialist since December 14th. I even got my nurse case manager on it, to no avail. Nobody was going to be able to see me until mid-January.
I happen to have an acquaintance who is a physician, as is her husband. It's the kind of relationship brought about by kids - our children are friends, so we see each other at birthday parties, volunteering at school, field trips, etc. We are very friendly but not good friends; she's been very busy working, as have I, and except for our children (who are now both A+ students in a rigorous IB program), we are in different social circles.
Another friend who knows both of us told me I should tap her as a resource to get seen quicker.
Now, normally I'm not shy, and would do that. I've done it with different people in other capacities. But, she is going through something worse than I'm going through - her son - my son's friend since 3rd grade - has a serious disease and spends a lot of time in the hospital. So, of course I know she has other things on her mind, and no way am I going to bother her.
Yesterday though, she called me. She'd heard about my situation and wanted to help. 30 minutes after the phone call, I had an appointment with a specialist - for this morning.
I just got home.
I'm not bitter, this is the world we live in. It isn't what you know/how sick you are. Who you know is the most important thing in any endeavor.
Anyway, the doctor said several interesting things. First, in his 20 years of practice, he had never seen a case of c-diff as bad as mine where the person didn't end up losing their colon or their life (or both). He looked at me in amazement. I was the worst he'd ever seen.
He said my gallbladder was the size of a melon on the hospital scans. (I don't know what that means).
He also is concerned that I am still not well and thinks I possibly have a bowel perforation and/or abscess.
So, it's not over yet.
They are arranging for another abdominal CT scan, STAT.
STAT, I'm sure, means sometime after the holidays when folks get around to it.
He apologized for my having to have more radiation. It was my turn to look at him in amazement. I said, "Oh, don't worry, the cancer will get me long before radiation does."
I asked him what would be the "cure" for a perforation or abscess and he said they would put tubes in to drain it, and it didn't necessarily mean surgery, which eased my mind a bit. I've been living in fear of shitting into a bag for over a month now, and I apologize to any of you readers who have stomas. I just don't think I could do it.
Of course, that isn't true, is it? The human capacity for putting up with what we thought we couldn't knows no end. I imagine if I had to have a stoma, I would handle it as I did everything else - probably with a lot of poop jokes.
He also said c-diff comes back in 7 days, "like clockwork." He wants me to finish my vancomycin, (last one today) and then, just ..... wait.
7 days from now is the 29th. He said, "that'll get you through the holidays."
That frightens me beyond measure. I know for a fact I won't survive another bout of c-diff like I had before. And, the doctor seemed pretty amazed I survived it the first time. Unfortunately, I can't live on antibiotics forever so I have to stop.
But, I have refills and I'm refilling them. At the slightest change - a loose BM, a new pain, a funny feeling, I'm starting up again. The fear of c-diff is a lot stronger than any doctor's opinion, and there is still no certainty that I am over it. If my bowel is, indeed, perforated, than it seems like stopping the antibiotics would be a bad idea. But, I don't have an MD so I will trust what he says.
For now.
I happen to have an acquaintance who is a physician, as is her husband. It's the kind of relationship brought about by kids - our children are friends, so we see each other at birthday parties, volunteering at school, field trips, etc. We are very friendly but not good friends; she's been very busy working, as have I, and except for our children (who are now both A+ students in a rigorous IB program), we are in different social circles.
Another friend who knows both of us told me I should tap her as a resource to get seen quicker.
Now, normally I'm not shy, and would do that. I've done it with different people in other capacities. But, she is going through something worse than I'm going through - her son - my son's friend since 3rd grade - has a serious disease and spends a lot of time in the hospital. So, of course I know she has other things on her mind, and no way am I going to bother her.
Yesterday though, she called me. She'd heard about my situation and wanted to help. 30 minutes after the phone call, I had an appointment with a specialist - for this morning.
I just got home.
I'm not bitter, this is the world we live in. It isn't what you know/how sick you are. Who you know is the most important thing in any endeavor.
Anyway, the doctor said several interesting things. First, in his 20 years of practice, he had never seen a case of c-diff as bad as mine where the person didn't end up losing their colon or their life (or both). He looked at me in amazement. I was the worst he'd ever seen.
He said my gallbladder was the size of a melon on the hospital scans. (I don't know what that means).
He also is concerned that I am still not well and thinks I possibly have a bowel perforation and/or abscess.
So, it's not over yet.
They are arranging for another abdominal CT scan, STAT.
STAT, I'm sure, means sometime after the holidays when folks get around to it.
He apologized for my having to have more radiation. It was my turn to look at him in amazement. I said, "Oh, don't worry, the cancer will get me long before radiation does."
I asked him what would be the "cure" for a perforation or abscess and he said they would put tubes in to drain it, and it didn't necessarily mean surgery, which eased my mind a bit. I've been living in fear of shitting into a bag for over a month now, and I apologize to any of you readers who have stomas. I just don't think I could do it.
Of course, that isn't true, is it? The human capacity for putting up with what we thought we couldn't knows no end. I imagine if I had to have a stoma, I would handle it as I did everything else - probably with a lot of poop jokes.
He also said c-diff comes back in 7 days, "like clockwork." He wants me to finish my vancomycin, (last one today) and then, just ..... wait.
7 days from now is the 29th. He said, "that'll get you through the holidays."
That frightens me beyond measure. I know for a fact I won't survive another bout of c-diff like I had before. And, the doctor seemed pretty amazed I survived it the first time. Unfortunately, I can't live on antibiotics forever so I have to stop.
But, I have refills and I'm refilling them. At the slightest change - a loose BM, a new pain, a funny feeling, I'm starting up again. The fear of c-diff is a lot stronger than any doctor's opinion, and there is still no certainty that I am over it. If my bowel is, indeed, perforated, than it seems like stopping the antibiotics would be a bad idea. But, I don't have an MD so I will trust what he says.
For now.
Monday, December 19, 2011
c-Diff - Update
Most people recover from C-Diff in 3 to 10 days. As you all know by now, I am not most people. It has been very disheartening being sick as long as I have been - since Thanksgiving - but last weekend, I saw an uptick in my health and now I believe I am on a (very long) road to recovery.
My life, since I got out of the hospital on December 3rd has been this:
1. Mornings about 9:30: Painfully and oh, oh so slowly, I get out of bed. My colon hurts, and is swollen, and I am carrying a 9 months pregnant-sized belly around. My feet were also swollen and I weighed 118 pounds out of the hospital - 18 pounds more than when I went in, and that was before constant diarrhea and 9 days of no eating, so I'm clearly extremely bloated. Sitting up is like climbing a mountain with broken ribs, and trying to put my feet on the floor is like finding a crevice and having to push around to find solid ground.
For a while, I decided to sleep on the couch as I could not breathe lying down in bed. Then I got out a sloped wedge pillow I had and was able to sleep propped up. My husband wanted me next to him, maybe to keep an eye on me.
2. After the difficulty of getting out of bed, I forced myself to sit at the dining table and have a half cup of decaf coffee and read the paper. This has been my routine for 18 years, and I wanted that normality. This was very painful for several reasons: sitting up straight is extraordinarily difficult on whatever was going on inside with my colon; I'd lost a significant amount of weight and my hard wooden chairs are painful on my butt/back bones, and I have been experiencing neurological problems, so each turn of the head, or eyes, or slight movement, sends electrical shocks down my body that I can actually hear. It sounds like the whooshing wind. I force myself to eat a Fage yogurt and read for as long as I can.
3. Hobble to the bathroom and release toxins.
Many times.
4. Wash hands and retrieve (slowly and gently) my iPhone and iPad, and head (slowly, hunched, and shuffling) toward the couch. I had it set up with a small table next to it, a 10 foot Apple charger, a glass of water, pain meds, several pillows for propping, and a blankie. There I would spend the remainder of the day - until bedtime. My habit has been to watch documentaries on Netflix (saw some good ones too) and then read for a while with my iPad kindle app, then watch some more documentaries. I'm reading a book a day, and I'm a picky reader. Ten bucks a day is a lot to spend, so I'm trying to find more movies or books that last longer. (Suggestions welcome but I am looking for good literature or interesting non-fiction - I like memoirs of non-famous people. I don't like mysteries or popular formulaic fiction - and definitely not science fiction.)
5. Take a bath. (Showers require too much standing up but I have a removable showerhead for washing hair.)
Up until last weekend, that was all I could do. I didn't want to talk on the phone - or in person - because breathing was difficult. Moving was difficult. Living was difficult. I couldn't answer email (I'm sorry) as it required more energy or thought than I could muster.) I felt that my colon was still in danger of rupture. I was very, very sick in a way I had not been before and in a way I find hard to describe. "Just snap out of it!" Impossible.
My husband stayed home for a week from work, because I couldn't stand long enough to make myself some soup, and it hurt terribly to get more water or move around. I was extremely tired, slightly depressed and feeling like I was never going to come out of this disease. The second week, my husband had to go back to work so I was alone. By then, I could stand long enough to make soup and mostly, I didn't think I would die right then so it was okay for him to be gone all day. But, it was lonely and I thought this bed to couch existence would be my life until cancer got me.
We had no Christmas tree - my family didn't want to get it without me. I understand that, but it was a burden on me to know that without me, they wouldn't celebrate Christmas. We have all decided that after the holidays (when they are on sale) we will get an artificial tree. As much as we love real trees, there may be times in the future when I can't leave the house again and they need to celebrate the holiday. We can still get a real tree and choose the best as a family but if I'm sick, we can pull down the fake one.
And, you'll note my optimism in planning to be around for another Christmas. But, I no longer feel that is a certainty.
Eventually, the diarrhea slowed. I was able to get around a bit better. I could do a load of laundry, walk to the kitchen. The bad pain went from all over my midsection to just the right lower quadrant. It feels a lot like the pain you get when you run too hard and get that stitch, only mine doesn't go away. The rest of my abdomen feels like I did a hundred sit-ups.
All the water weight from the hospital is gone and I weigh 90 pounds. My stomach is very deformed but I'm not 9 months pregnant anymore - now it's like like I have an alien baby - a big swelling here, a concave area there, a tail-sized length over here. The diarrhea has slowed to just a few times a day.
Two days ago, I got dressed for the first time.
This Saturday, I was able to walk long enough to get a Christmas tree. I was nauseated when I got home, but I did it. We decorated it yesterday.
Thank goodness for Amazon Prime. I have almost all my Christmas shopping done. I have to go to one store, which will be an adventure and I'm not sure I can.
I'm still trying to get an appointment with a specialist, although they are saying 3 weeks, which is completely unacceptable. I saw a Dr. Nassir in the hospital and some sort of protocol means I have to see him again and he's not available. I don't understand this because the woman on the phone told me there were 40 infectious disease specialists in their practice, and I don't care which one I see. I saw Nassir in the hospital for maybe a minute and he only directed my care until the hospitalist took over. I no longer feel like my colon is in danger of rupturing anymore but I am still taking vancomycin (my PCP kindly gave me six refills) and I want to know if I can stop taking it, what to do if the c-diff comes back, how long I'll be in this debilitated state, why it has taken me weeks to recover when others only take days, when I can eat a normal diet and when I can start chemo. I told the appointment-setting woman on the phone to please call me Monday and if she couldn't get me an appointment in a reasonable time I'd go elsewhere.
So far, it's almost 1:00 and no call.
I've had a home health nurse calling me, and they said they were going to send somebody out, but they changed their minds. That's fine with me as I don't know what a nurse could do for me, but I just called her to see if she can help me get in to see a doctor quicker.
This has been an awful disease and it's frightening being as sick as I was, and I don't think I'll ever be able to relate my hospital experience online - it was the worst thing I've ever gone through. Having sepsis and never-ending diarrhea is not the way I want to go out, I can tell you that much. I'm glad I'm recovering but I have had to tell my work I won't be back when I was supposed to in January, and now my money will run out. My job is only protected for a few more months and I'm not sure I'll make it back.
And, I've had to miss chemo, which makes me very afraid the surgery I had to remove my liver was for nothing. We all know that metastatic cancer means there are cancer cells in other places, and without chemo to kill it I may end up right where I started, only this time without the hope of surgery.
But, I'm stepping on the path to recovery, however temporarily, and the flowers alongside that path are lovely. I'm able to function now, although at a very reduced ability, but it's better than I was two weeks ago, and I hope two weeks from now I'll have even more recovery behind me. I'm so thin no clothes fit and I look scary but I hope to gain that weight back soon.
This disease left me with the knowledge that I'm very vulnerable. I thought, in a cavalier way, that the liver resection surgery would surely give me years and years and I'd eluded death, at least in the short term. I thought I might see my son go to college, my other son get married, maybe even see a grandchild. I know now that isn't close to a guarantee, nor is it likely. The life expectancy for a person with metastatic breast cancer to the liver is 2 years, and it is no longer impossible to believe that I will be gone next year. It's made me sad and while I have not given up the fight, I know know there are powers beyond your will, mind and desire that are stronger than you are.
C-diff may not kill me in the conventional way, but since I can't do chemo, if I die of cancer in the next year, it will certainly have played a role.
Wednesday, December 7, 2011
C-Diff
This will be short but I finally can sit up and write a quick blog post, so I will let you all know what is going on.
Thanksgiving evening I took a neupogen shot, which gave me a bad reaction as it often does. I spent that night in severe agony, feeling like I was delivering a baby out of my spinal canal. The pain eased up by the next day but I never recovered, I stayed in bed nearly unconscious and sick for two days. Saturday night, diarrhea started and I checked my temperature: 101.7. I'm supposed to call my oncologist anytime my fever goes above 100.5 so I called, and they told me I probably had neutropenic fever and to get to the ER and they would call to have me admitted.
I can't possibly describe what I went through from that point on. Hellish would be an understatment and the worst experience of my life would not. I didn't have neutropenic fever, I had a SuperBug infection called C-Diff. (Clostridium difficile) By the time I got there, I was in a bad way. I had fulminent c-diff colitis and was septic. I spent two nightmarish days in ICU with a dysentery-like diarrhea, pain,, and sickness like I've never felt before. My heart rate was 160 and my blood pressure sky high. They gave me antibiotics.
The antibiotic started to work, so they moved me to a ward, on IV flagyl and vancomycin. They told me they thought they would have to take my entire colon out, although I was in such bad shape they didn't want to operate on me, and in looking it up, survival is not good for that operation.
On about Day Four the surgical team decided I'd recovered enough that my colon was safe, and I was so relieved. But, right at that point is where my recovery stopped. And, my belly started growing. On the seventh day they let me out of the hopsital with a prescription for vancomycin and I went home.
I've been home since Friday, and today is Wednesday. At first, I was overloaded with IV fluids. My legs were swollen from thigh to ankle and they looked like elephant trucks. My stomach was also very bloated, and I also thought that was from IV fluids. Made it very hard to breath. But, now that the IV fluids are gone, my stomach is still horribly distended. I can do only the most basic self-care; my husband had to take the week off to help me. I still have diarrhea about 8 times a day and I don't seem to be improving.
My last meal was Thanksgiving - on that date I weighed about 100 pounds. When I got out of the hospital that first day, after non-stop diarrhea and no food, I weighed 118. Now I weigh 110.
I saw my Primary Care Physician yesterday and he said that if I wasn't better in 24 hours, he wanted to re-admit me to the hospital. My vitals are fine but the belly distension is worrisome. I'm not better but I made an appointment with my oncologist for tomorrow, and I'll see what he says. I know he'll fight the bowel removal and I want him in charge of my care. So, between these two doctors, I'll likely be back in the hospital this weekend but hopefully they will have a trick or two up their sleeve to get me into a real recovery.
I have not been able to lift anything heavier than an iPad or iPhone and can't update the blog from those devices. I tried to give twitter updates and will continue to do that when I can't post.
I know there have been many worried thoughts about me, many prayers sent up, and well-wishes sent my way.
Thank you for that, and keep them up for I'm not out of the woods yet. All I want now is a nice, simple Christmas with my family without the fear of losing my colon hanging over my head!
Thanksgiving evening I took a neupogen shot, which gave me a bad reaction as it often does. I spent that night in severe agony, feeling like I was delivering a baby out of my spinal canal. The pain eased up by the next day but I never recovered, I stayed in bed nearly unconscious and sick for two days. Saturday night, diarrhea started and I checked my temperature: 101.7. I'm supposed to call my oncologist anytime my fever goes above 100.5 so I called, and they told me I probably had neutropenic fever and to get to the ER and they would call to have me admitted.
I can't possibly describe what I went through from that point on. Hellish would be an understatment and the worst experience of my life would not. I didn't have neutropenic fever, I had a SuperBug infection called C-Diff. (Clostridium difficile) By the time I got there, I was in a bad way. I had fulminent c-diff colitis and was septic. I spent two nightmarish days in ICU with a dysentery-like diarrhea, pain,, and sickness like I've never felt before. My heart rate was 160 and my blood pressure sky high. They gave me antibiotics.
The antibiotic started to work, so they moved me to a ward, on IV flagyl and vancomycin. They told me they thought they would have to take my entire colon out, although I was in such bad shape they didn't want to operate on me, and in looking it up, survival is not good for that operation.
On about Day Four the surgical team decided I'd recovered enough that my colon was safe, and I was so relieved. But, right at that point is where my recovery stopped. And, my belly started growing. On the seventh day they let me out of the hopsital with a prescription for vancomycin and I went home.
I've been home since Friday, and today is Wednesday. At first, I was overloaded with IV fluids. My legs were swollen from thigh to ankle and they looked like elephant trucks. My stomach was also very bloated, and I also thought that was from IV fluids. Made it very hard to breath. But, now that the IV fluids are gone, my stomach is still horribly distended. I can do only the most basic self-care; my husband had to take the week off to help me. I still have diarrhea about 8 times a day and I don't seem to be improving.
My last meal was Thanksgiving - on that date I weighed about 100 pounds. When I got out of the hospital that first day, after non-stop diarrhea and no food, I weighed 118. Now I weigh 110.
I saw my Primary Care Physician yesterday and he said that if I wasn't better in 24 hours, he wanted to re-admit me to the hospital. My vitals are fine but the belly distension is worrisome. I'm not better but I made an appointment with my oncologist for tomorrow, and I'll see what he says. I know he'll fight the bowel removal and I want him in charge of my care. So, between these two doctors, I'll likely be back in the hospital this weekend but hopefully they will have a trick or two up their sleeve to get me into a real recovery.
I have not been able to lift anything heavier than an iPad or iPhone and can't update the blog from those devices. I tried to give twitter updates and will continue to do that when I can't post.
I know there have been many worried thoughts about me, many prayers sent up, and well-wishes sent my way.
Thank you for that, and keep them up for I'm not out of the woods yet. All I want now is a nice, simple Christmas with my family without the fear of losing my colon hanging over my head!
Thursday, November 24, 2011
Happy Thanksgiving
Surviving a long difficult winter, the Pilgrims - what was left of them anyway - had a feast. 101 men, women and children had arrived to the New World in December, during a winter so harsh that it had killed fully half of them - only 53 remained. Despite their grief, in the spring, those who had lost children or parents still planted crops with hopes for their future. They got advice from Native Americans, who showed them how to use fish as fertilizer. And, when harvest season came around, they did what Americans do so well, and decided to have a feast. 90 Wampanoag Indians came, bringing deer, fish and other goodies, and the Pilgrims harvested their crops, and together they ate and sang and joined together in celebration of life. And, I like to think somebody dredged up a pie somewhere.
Or two.
They didn't sit around wailing for all they had lost, complaining about the hardships they had endured. They took time to gave thanks for what they had and planned to better in the future. This Thanksgiving holiday, declared by none other than Abraham Lincoln in the middle of the Civil War, is about being grateful in spite of adversity, enjoying and sharing your bounty with the friends who share life with you, and the human ability to look ahead to what is better.
In a way, Thanksgiving is a holiday tailor-made for the cancer patient. The year was full of struggles and hard times, and not just for me. Many of us can no longer do the things we used to find easy. Some have already suffered losses, and some wonder if this is their last Thanksgiving. Others have completed treatment but now fear cancer will rear its ugly head sometime on the road ahead. But, here we all are, on a day dedicated to Thanksgiving. We can take a step back and remind ourselves of all we have still, while enjoying a delicious meal with family and friends and with hope bright for the future, however long that may be.
Happy Thanksgiving Everybody. Save me a piece of pie.
Wednesday, November 23, 2011
Recovering from Liver Resection Surgery
Thank you all so much for your comments on my article at empowerHER. The fact that you took the time to comment is every bit as heartwarming as the applause I wrote about was. Now, on to your regularly scheduled posting.
I expected to recover from surgery like a rock star, and that's exactly what I did. Lots of narcotics, sleeping until noon, hanging out with groupies.
Well, maybe not that last part.
I started to feel guilty. Very kind people were bringing me delicious foods so I didn't have to cook, and while it did hurt to stand up, (due to the fact that they seem to have sewn the top of my stomach to the bottom of it, leaving me with the posture of a hunchback) I was feeling so good I knew I could have managed a meal if I'd had to.
I guess I wasn't thinking that I shouldn't be on my feet, even if I could be.
What, me? Rest?
I had heard that people who have liver resections feel exhaustion like nothing else can cause; that they sleep for hours and days and never feel rested, and that doing something simple like taking a shower takes all their energy for the day.
I scoffed. That's for other people, not for a diva like me.
Once the pain was gone (on day three) I felt fine. I was sure I would be going back to work long before my due date of December 5th. I was thinking somebody should draw a comic book about me. I could be a super hero called Recovery Woman. Nothing could keep me down! In the past, Recovery Woman had gone furniture shopping four days after an appendectomy and had scars that appeared healed almost before leaving the hospital. Even though this was the biggest surgery I'd ever have, I seemed to be following my pattern - miraculous recovery. As people would come by to check on me, I was almost embarrassed at how well I was doing.
Then, two weeks after surgery, I crashed. I suddenly had difficulty breathing Not acute, not dangerous, just very, very uncomfortable. I felt very short of breath all the time, like you feel after you blow up balloons, only the party never ends. The exhaustion hit me, and I slept through alarm clocks - not one alarm clock, and not two, but three. I slept like a teenage boy who has an essay due. I slept like a cat in a sun spot on a windy fall day. I slept like Snow White after she bit the apple. My sleep was impenetrable by any outside force. Combine that with my shortness of breath, and my life suddenly became about struggle rather than recovery.
I had my three week post-op with my surgeon, and told him about my shortness of breath. He did a chest x-ray, which came back "pristine." We both then assumed I was anemic and my oncologist would check for that. I soon began chemo again, and told my oncologist about it. My blood tests were good, and he became alarmed and thought perhaps it was a clot, and so ordered an immediate angiogram, and I wasn't allowed to leave until the results came back.
No clot.
Unfortunately, that meant no diagnosis.
A couple of days ago, the pain became acute. It almost feels like I have appendicitis again, only I don't have an appendix anymore, and truthfully, this is much milder. So far. It's very low in my abdomen, possibly colon, but it's on both sides. I just have to live with it and hope it goes away as part of the healing process. If this pain doesn't go away by next week though, I am going to have to address it.
Aside from this sudden pain, something as strenuous as reading is exhausting and leaves me breathless and dizzy. I occasionally have to take a big, deep and painful breath, just to get back on track. Talking on the phone - actually, talking, in general, is very difficult. You can't talk and blow up balloons at the same time.
And, when it rains.......My shoulder had begun hurting me again, and so I went back for another cortisone shot (yes, it's still frozen, and yes, it likely be for the rest of my life at this point - but with cortisone shots I can get pain relief and 75% of my movement back). I told the PA about the shortness of breath, and he suggested that maybe the diaphragm was inflamed from the surgery. The diaphragm and liver are right next to each other, and whether that can happen I don't know; whether it would have shown up on the angiogram or the x-ray, I also don't know. It makes sense to a layman, maybe it wouldn't to a doctor. But, the acute pain is in the lower abdomen - very low. So, who knows?
And, because no post by me would be complete without mentioning pee, I seem to have a constant bladder infection - minus the infection part. Friends have suggested interstitial cystitis, which makes sense, and I suppose could be causing this lower abdominal pain. Or not.
So, here I sit in front of my computer, post-surgery. Breathless, exhausted, needing constant naps, yelping in pain when I pee, needing to pee all day, lower abdomen burning and aching and stabbing me if I move, especially in the classic "put your knee to your chest" position.
All those leftover pain meds from healing so fast? They are almost gone.
After talking to my doctor last week, I decided to take an extra month off work, because I'm not good to anybody right now. Hopefully, at the very least, I will at least have more energy by January, when I have no choice but to go back or starve. But, I hope that I feel much better, especially whatever is going on in my lower abdomen.
Aside from all that, I'm grateful I made it through surgery and I've got this chance to get healthy. Nobody promised me it would be easy, and as it turns out, it isn't. I'm sure whatever is going on can all be fixed. It'll just mean more tests, more waiting rooms, more poking. Pain or no, I think I'll wait until after the holiday.
So, I guess I healed like a rock star - an aging, overdone, used up rock star.
I expected to recover from surgery like a rock star, and that's exactly what I did. Lots of narcotics, sleeping until noon, hanging out with groupies.
Well, maybe not that last part.
I started to feel guilty. Very kind people were bringing me delicious foods so I didn't have to cook, and while it did hurt to stand up, (due to the fact that they seem to have sewn the top of my stomach to the bottom of it, leaving me with the posture of a hunchback) I was feeling so good I knew I could have managed a meal if I'd had to.
I guess I wasn't thinking that I shouldn't be on my feet, even if I could be.
What, me? Rest?
I had heard that people who have liver resections feel exhaustion like nothing else can cause; that they sleep for hours and days and never feel rested, and that doing something simple like taking a shower takes all their energy for the day.
I scoffed. That's for other people, not for a diva like me.
Once the pain was gone (on day three) I felt fine. I was sure I would be going back to work long before my due date of December 5th. I was thinking somebody should draw a comic book about me. I could be a super hero called Recovery Woman. Nothing could keep me down! In the past, Recovery Woman had gone furniture shopping four days after an appendectomy and had scars that appeared healed almost before leaving the hospital. Even though this was the biggest surgery I'd ever have, I seemed to be following my pattern - miraculous recovery. As people would come by to check on me, I was almost embarrassed at how well I was doing.
Then, two weeks after surgery, I crashed. I suddenly had difficulty breathing Not acute, not dangerous, just very, very uncomfortable. I felt very short of breath all the time, like you feel after you blow up balloons, only the party never ends. The exhaustion hit me, and I slept through alarm clocks - not one alarm clock, and not two, but three. I slept like a teenage boy who has an essay due. I slept like a cat in a sun spot on a windy fall day. I slept like Snow White after she bit the apple. My sleep was impenetrable by any outside force. Combine that with my shortness of breath, and my life suddenly became about struggle rather than recovery.
I had my three week post-op with my surgeon, and told him about my shortness of breath. He did a chest x-ray, which came back "pristine." We both then assumed I was anemic and my oncologist would check for that. I soon began chemo again, and told my oncologist about it. My blood tests were good, and he became alarmed and thought perhaps it was a clot, and so ordered an immediate angiogram, and I wasn't allowed to leave until the results came back.
No clot.
Unfortunately, that meant no diagnosis.
A couple of days ago, the pain became acute. It almost feels like I have appendicitis again, only I don't have an appendix anymore, and truthfully, this is much milder. So far. It's very low in my abdomen, possibly colon, but it's on both sides. I just have to live with it and hope it goes away as part of the healing process. If this pain doesn't go away by next week though, I am going to have to address it.
Aside from this sudden pain, something as strenuous as reading is exhausting and leaves me breathless and dizzy. I occasionally have to take a big, deep and painful breath, just to get back on track. Talking on the phone - actually, talking, in general, is very difficult. You can't talk and blow up balloons at the same time.
And, when it rains.......My shoulder had begun hurting me again, and so I went back for another cortisone shot (yes, it's still frozen, and yes, it likely be for the rest of my life at this point - but with cortisone shots I can get pain relief and 75% of my movement back). I told the PA about the shortness of breath, and he suggested that maybe the diaphragm was inflamed from the surgery. The diaphragm and liver are right next to each other, and whether that can happen I don't know; whether it would have shown up on the angiogram or the x-ray, I also don't know. It makes sense to a layman, maybe it wouldn't to a doctor. But, the acute pain is in the lower abdomen - very low. So, who knows?
And, because no post by me would be complete without mentioning pee, I seem to have a constant bladder infection - minus the infection part. Friends have suggested interstitial cystitis, which makes sense, and I suppose could be causing this lower abdominal pain. Or not.
So, here I sit in front of my computer, post-surgery. Breathless, exhausted, needing constant naps, yelping in pain when I pee, needing to pee all day, lower abdomen burning and aching and stabbing me if I move, especially in the classic "put your knee to your chest" position.
All those leftover pain meds from healing so fast? They are almost gone.
After talking to my doctor last week, I decided to take an extra month off work, because I'm not good to anybody right now. Hopefully, at the very least, I will at least have more energy by January, when I have no choice but to go back or starve. But, I hope that I feel much better, especially whatever is going on in my lower abdomen.
Aside from all that, I'm grateful I made it through surgery and I've got this chance to get healthy. Nobody promised me it would be easy, and as it turns out, it isn't. I'm sure whatever is going on can all be fixed. It'll just mean more tests, more waiting rooms, more poking. Pain or no, I think I'll wait until after the holiday.
So, I guess I healed like a rock star - an aging, overdone, used up rock star.
Friday, November 18, 2011
Finding Support - and Support Me!
I have joined a network for women's health, called "EmpowerHer." It's a start-up that looks like it could be fantastic way to meet up with others who have your health condition or concerns. There is already a group for breast cancer, with a nurse who will respond to medical questions, and I intend to participate there and help newbies with my non-medical advice. I also started a group myself, for metastatic breast cancer patients, so if you have an interest in talking to others with metastatic cancer, either as a patient or caregiver, feel free to join up. We can talk about anything we want.
Now, my subject line says you can support me, and I know you want to. So how? Well, they are running a contest on their site. I share a story, get the most comments, and the most page views, and I win money.
I like money!
I like money a lot!
So, I wrote you a nice, true, short story, about what happened to me yesterday when I walked into work for the first time since early October. It's all heart-wrenching and stuff, and I would have posted it here on my own blog (and added 400 more words probably) but I can't run a contest for myself.
http://www.empowher.com/community/share/finding-support
After you read it, please leave a comment about where you found support when you were diagnosed, or how you as a caregiver do something to support your loved one with cancer or anything you want really because it's the most comments, not the best or most relevant. I think you can leave an anonymous comment, although they won't spam you if you register.
And, thank you in advance for helping me right before Christmas, and for being part of my support network. Because, my blog readers, you are a huge part of my support network. I am not sure I could do this without you all rooting me on from afar.
Anyway, lots of other bloggers will be entering so let's show everybody my readers are the best!
Thank you!
Now, my subject line says you can support me, and I know you want to. So how? Well, they are running a contest on their site. I share a story, get the most comments, and the most page views, and I win money.
I like money!
I like money a lot!
So, I wrote you a nice, true, short story, about what happened to me yesterday when I walked into work for the first time since early October. It's all heart-wrenching and stuff, and I would have posted it here on my own blog (and added 400 more words probably) but I can't run a contest for myself.
http://www.empowher.com/community/share/finding-support
After you read it, please leave a comment about where you found support when you were diagnosed, or how you as a caregiver do something to support your loved one with cancer or anything you want really because it's the most comments, not the best or most relevant. I think you can leave an anonymous comment, although they won't spam you if you register.
And, thank you in advance for helping me right before Christmas, and for being part of my support network. Because, my blog readers, you are a huge part of my support network. I am not sure I could do this without you all rooting me on from afar.
Anyway, lots of other bloggers will be entering so let's show everybody my readers are the best!
Thank you!
Monday, November 14, 2011
I Left My Lobe in San Francisco: Liver Resection Story. Going Home
I was weaned off the epidural machine. I was eating delicious foods such as orange jello and pea soup. I was walking myself to the bathroom, and my pain level was only a 2 or 3.
It was Saturday, October 8th, and it was time to go home.
There was one more hurdle to get through, and that was the drive from San Francisco to Sacramento. Now, I don't want to make this a political blog, but let's just say our legislature, probably like yours, has found many things to spend our tax dollars on that they believe are more important than improving crumbling roads. As an example, they are allocating several billion dollars on this new, super-modern technology (a train), which is designed to get people from one part of California that nobody goes to, to another part of California that nobody goes to. Fixing the roads between the biggest city in California and the Capitol of the state is not important compared to laying tracks from Bakersfield to Palmdale.
Hey, those cows need something to look at.
In short, our freeways are in deplorable shape. In the 100 miles between the hospital and my house, there are 877,423 bumps in the road. And, those are the large ones.
I know. I counted.
On the way there.
Why? I was terrified of coming home and had been from the beginning. Who wouldn't be? In my condition, I could go over one of California's legendary potholes, hit a large bump, my stitches could slam open and my guts spill out, right onto my lap.
My favorite show in the world right now is the Walking Dead. But, I like it from the comfort of my couch, with its gore causing my stomach to churn, from inside my skin, where it belongs.
I was not the only one afraid of the ride home. My husband was also quite nervous. Let's just say we have the same relationship that your grandparents had. He doesn't drive the right way, and I tell him so. So he knew he was going to have to hear about each one of the 877,423 bumps, and be told 877,423 times that he should take them smoother.
And he was, of course, right.
For once.
To protect us both, like you all would, I made a plan. In the trunk of my husband's car there were a bunch of pillows I'd brought from home to prop myself up and protect myself from California's neglect. I also brought one of those foam mattress pads - you know the kind with the eggshell bumps everywhere? I figured I could line the back seat with that, prop myself with pillows and soften some of the major bumps and maybe even take a nap. At the very least, I could flip through a magazine and try to ignore what was going on from my padded cell.
But, that wasn't all. For the rest of the plan to work, I needed an accomplice: my nurse. What I wanted to do was get my final shot of dilaudid and take a valium right before I was released. Since the shot is supposed to last two hours and the valium seemed to relax me for at least that, I figured I could avoid the pain of the ride entirely by being drugged.
Hell, why not? Half of Californians do it.
The nurse, whose name I forget but who was with me for three days, thought I was being a bit silly but she got on board. She'd been absolutely wonderful the entire time and the instant I remember her name I will send her a thank you card. Anyway, she either had never driven across California or thought I was a wimp (or both), but she readily agreed to my plan. I was still allowed to have medication, so why not?
It sometimes seems checkout in the hospital is endless, but they have it down to a science at UCSF and the entire thing took less than an hour. In fact, they came in to remove my IV, and I had to ask them to wait as I wanted to use it one more time for the medicine.
Now, you have heard a lot about pee in my little hospital saga and I am afraid I'm going to give you one more squirt. If you haven't been squeamish or Miss Mannerish about this so far, this one won't bug you. But, if you have shaken your head and said, 'Ann, you are being very undignified," than I suggest you skip the next few paragraphs.
Getting ready for a two hour car ride means you use the rest room. Even though I was being released, I was still using the measuring cup they slip inside the toilet, so I sat properly and did my thing, no problems anymore. And, when I saw what I left inside the cup, visions of the Walking Dead came floating back to my mind. Inside that cup was a brown liquid. Not a light, yellow brown. But a deep, gritty brown, with chunks in it. Like dirt mixed with sand mixed with danger.
I was shocked. What the hell was that? Did that come out of me? Were they doing construction somewhere and dirty stuff from pipes spilled into the cup? I actually looked up to see if there was a leak above my head. Were pieces of what was left of my liver breaking off and coming through my urethra?
Was that something that was going to prevent me from going home? Oh no! As afraid of the car ride as I was, I wanted out of the hospital! Yes, I expected a difficult two hours, but after that, I would be sleeping in my own bed, petting my own dog, hugging my own sons (who had left days ago) and be in my own, comforting environment.
Now what? Do I tell somebody? Do I leave it there for them to notice after I am released and they are cleaning the room?
What would they think that was? Would they call me back?
The nurse came in to tell me that a doctor was on her way in to remove my staples and put on tape to hold me closed. I shamefully told her about the brown, gritty pee.
She didn't seem to care. She said she'd look at it later.
Shortly, a med student came in with a staple remover, and I gallantly tried again. She also didn't care. Perhaps looking at coffee-colored pee is above their pay grades, or maybe they just wanted me out of there.
I didn't think I'd been that bad.
But, I knew they wouldn't let me die, or pee out my remaining liver in chunks, even if I had been annoying. It apparently wasn't an emergency, and I was clearly going home - so I forgot the pee and went back to worrying about the trip.
After I had a thousand pieces of tape placed on me in lieu of staples (that med student was definitely an over-achiever and a 7.5 earthquake wasn't going to open me up now) the nurse came back in, gave me my Valium, my shot of Dilaudid, took out my IV and wished me well. I thanked her for her compassionate care, and my husband went to pull the car around. I gathered my things and a few minutes later, the transport person with the wheelchair showed up, and I was off.
I was impressed. My husband had done a fantastic job of lining the backseat with the mattress pad and pillows, but being a woman, I changed my mind. I felt well enough to sit up straight and wanted to be in front. So, we grabbed some pillows, and I got in the car.
As we started driving through the city of San Francisco, the meds kicked in, and I began to doze off. Soon, I was fast asleep. At one point, we crossed from one interchange to another which had a large bump, and as we went over it, I woke up and said, "Ooohhhhhh" and then fell right back to sleep.
And, I slept pretty much until my husband pulled into our driveway. I had made one moan in 100 miles and 877,423 bumps, and that was it.
My plan had worked beautifully.
Pillows plus drugs equals no guts on the lap and no nagging of the husband. What could be better?
Well, yellow pee could be better.
Which is what happened when I got home. Whew.
It was Saturday, October 8th, and it was time to go home.
There was one more hurdle to get through, and that was the drive from San Francisco to Sacramento. Now, I don't want to make this a political blog, but let's just say our legislature, probably like yours, has found many things to spend our tax dollars on that they believe are more important than improving crumbling roads. As an example, they are allocating several billion dollars on this new, super-modern technology (a train), which is designed to get people from one part of California that nobody goes to, to another part of California that nobody goes to. Fixing the roads between the biggest city in California and the Capitol of the state is not important compared to laying tracks from Bakersfield to Palmdale.
Hey, those cows need something to look at.
In short, our freeways are in deplorable shape. In the 100 miles between the hospital and my house, there are 877,423 bumps in the road. And, those are the large ones.
I know. I counted.
On the way there.
Why? I was terrified of coming home and had been from the beginning. Who wouldn't be? In my condition, I could go over one of California's legendary potholes, hit a large bump, my stitches could slam open and my guts spill out, right onto my lap.
My favorite show in the world right now is the Walking Dead. But, I like it from the comfort of my couch, with its gore causing my stomach to churn, from inside my skin, where it belongs.
I was not the only one afraid of the ride home. My husband was also quite nervous. Let's just say we have the same relationship that your grandparents had. He doesn't drive the right way, and I tell him so. So he knew he was going to have to hear about each one of the 877,423 bumps, and be told 877,423 times that he should take them smoother.
And he was, of course, right.
For once.
To protect us both, like you all would, I made a plan. In the trunk of my husband's car there were a bunch of pillows I'd brought from home to prop myself up and protect myself from California's neglect. I also brought one of those foam mattress pads - you know the kind with the eggshell bumps everywhere? I figured I could line the back seat with that, prop myself with pillows and soften some of the major bumps and maybe even take a nap. At the very least, I could flip through a magazine and try to ignore what was going on from my padded cell.
But, that wasn't all. For the rest of the plan to work, I needed an accomplice: my nurse. What I wanted to do was get my final shot of dilaudid and take a valium right before I was released. Since the shot is supposed to last two hours and the valium seemed to relax me for at least that, I figured I could avoid the pain of the ride entirely by being drugged.
Hell, why not? Half of Californians do it.
The nurse, whose name I forget but who was with me for three days, thought I was being a bit silly but she got on board. She'd been absolutely wonderful the entire time and the instant I remember her name I will send her a thank you card. Anyway, she either had never driven across California or thought I was a wimp (or both), but she readily agreed to my plan. I was still allowed to have medication, so why not?
It sometimes seems checkout in the hospital is endless, but they have it down to a science at UCSF and the entire thing took less than an hour. In fact, they came in to remove my IV, and I had to ask them to wait as I wanted to use it one more time for the medicine.
Now, you have heard a lot about pee in my little hospital saga and I am afraid I'm going to give you one more squirt. If you haven't been squeamish or Miss Mannerish about this so far, this one won't bug you. But, if you have shaken your head and said, 'Ann, you are being very undignified," than I suggest you skip the next few paragraphs.
Getting ready for a two hour car ride means you use the rest room. Even though I was being released, I was still using the measuring cup they slip inside the toilet, so I sat properly and did my thing, no problems anymore. And, when I saw what I left inside the cup, visions of the Walking Dead came floating back to my mind. Inside that cup was a brown liquid. Not a light, yellow brown. But a deep, gritty brown, with chunks in it. Like dirt mixed with sand mixed with danger.
I was shocked. What the hell was that? Did that come out of me? Were they doing construction somewhere and dirty stuff from pipes spilled into the cup? I actually looked up to see if there was a leak above my head. Were pieces of what was left of my liver breaking off and coming through my urethra?
Was that something that was going to prevent me from going home? Oh no! As afraid of the car ride as I was, I wanted out of the hospital! Yes, I expected a difficult two hours, but after that, I would be sleeping in my own bed, petting my own dog, hugging my own sons (who had left days ago) and be in my own, comforting environment.
Now what? Do I tell somebody? Do I leave it there for them to notice after I am released and they are cleaning the room?
What would they think that was? Would they call me back?
The nurse came in to tell me that a doctor was on her way in to remove my staples and put on tape to hold me closed. I shamefully told her about the brown, gritty pee.
She didn't seem to care. She said she'd look at it later.
Shortly, a med student came in with a staple remover, and I gallantly tried again. She also didn't care. Perhaps looking at coffee-colored pee is above their pay grades, or maybe they just wanted me out of there.
I didn't think I'd been that bad.
But, I knew they wouldn't let me die, or pee out my remaining liver in chunks, even if I had been annoying. It apparently wasn't an emergency, and I was clearly going home - so I forgot the pee and went back to worrying about the trip.
After I had a thousand pieces of tape placed on me in lieu of staples (that med student was definitely an over-achiever and a 7.5 earthquake wasn't going to open me up now) the nurse came back in, gave me my Valium, my shot of Dilaudid, took out my IV and wished me well. I thanked her for her compassionate care, and my husband went to pull the car around. I gathered my things and a few minutes later, the transport person with the wheelchair showed up, and I was off.
I was impressed. My husband had done a fantastic job of lining the backseat with the mattress pad and pillows, but being a woman, I changed my mind. I felt well enough to sit up straight and wanted to be in front. So, we grabbed some pillows, and I got in the car.
As we started driving through the city of San Francisco, the meds kicked in, and I began to doze off. Soon, I was fast asleep. At one point, we crossed from one interchange to another which had a large bump, and as we went over it, I woke up and said, "Ooohhhhhh" and then fell right back to sleep.
And, I slept pretty much until my husband pulled into our driveway. I had made one moan in 100 miles and 877,423 bumps, and that was it.
My plan had worked beautifully.
Pillows plus drugs equals no guts on the lap and no nagging of the husband. What could be better?
Well, yellow pee could be better.
Which is what happened when I got home. Whew.
. Thank you for "liking" me on facebook. Keep it up!
Sunday, November 13, 2011
I Left My Lobe in San Francisco: Liver Resection Hospitalization - Vignette 5, 6 & 7
Shaking bed
Now, you might think a constant leg massage would be pleasant, but you'd be wrong. After a while, it's like that Vietnamese guy who gives you the massage after a pedicure and doesn't know when to stop. It goes on and on and the oil dries out and you are starting to feel bruised, but he's smiling up at you, saying, "You like?" thinking he's giving you special service, and wishing for a great tip. The hope in his eyes gives you no choice but to say yes. (And, to tip him well, which encourages him to bruise his next customer.)
These automated things are very annoying and every time you need to move, you can't because you are plugged into them. On Day Three, I'd had enough and took them off, and hid them from the nurses. I figured I was up and walking by then and wasn't going to clot. (I did the same with the nasal cannula for oxygen, another annoying piece of medical equipment.)
Unfortunately, I couldn't turn off my bed. Technology has come a long way, baby, and along with the compression stockings for your leg, your entire bed can act as a clot preventer.
My bed shook chronically, like a laughing Santa and his bowl full of jelly, except that I wanted to kill him, and I would never kill Santa. It went left, right, vibrated, jiggled, up and down and back again. It was near impossible to get comfortable in that bed and it was loud too. As soon as I'd find a comfortable position, the bed would jiggle and move me to the left, and I'd slide down, right onto my catheter tubing, right on to the epidural wire, causing a jolt of pain. I used pillows to try to prop myself in the same position despite the movements of the bed, but it was too difficult. The jarring of the bed moved the pillows, so you ended up at its mercy, like being rocked in a sailboat and not being able to stop the water.
Then came the time when it malfunctioned. Suddenly, it was acting like it was possessed - like the exorcist. Not only would it jiggle up, it would actually go up a few feet, as if I'd pushed the button to sit up. This was quite jarring at 2:00 a.m. It would do this for a few minutes then stop. I told the nurses, who didn't believe me, and dialed back my medication. It never happened when they were around, of course. Once, my husband saw it and we complained again. This time, the nurse believed us and called somebody in, who pushed some button and it stopped. Well, it didn't entirely stop, the bed still did its vibration thing. But, the ghosts went away.
Weaning off the Epidural
I was starting to be able to get through a cup of tea, some oatmeal and soup. And jello, which I never liked, but which is spectacular in a hospital; even the green. My food intake meant it was time to wean off the epidural and start on oral pain meds. The epidural had delivered a steady amount of pain killing medication directly into my spinal canal, and I could add more every 15 minutes. This was my main pain control after the operation, and now it was day five and I felt good.
I was, frankly, terrified.
I was attached to that machine like an umbilical cord, and I felt it gave me everything a real umbilical cord would: safety, comfort, and in my mother's case, a few mind-altering substances. (It was the 50s: martinis, cigarettes, and pregnancy was apparently a normal mix.) I knew if they took me off it, I would end up in agony, suffering, feeling the lack of a liver and the slicing of each broken muscle. I fantasized about taking it home with me, wondering how we'd refill it, or even get it in the car. But it was just a fantasy - not to be. I had to get off it and I knew that. I wanted out of there and was thinking home was a good place to be.
The anesthesiologist told me that they would lower it little by little, all day long. I would still be able to press the button for extra pain meds but the amounts delivered would be smaller. Depending on how I did, by the end of the night I'd be off it.
"Are you ready?"
I had no choice. So, at about 10:00 am they dialed it down.
I didn't notice.
About an hour later, they lowered it some more. Again, I didn't notice. That went on until about half way through the day, when the pain increased a bit, and I asked for pain meds, which they gave. The continued to lower the numbers and I continued to do well, and by 6:00 that evening, I was on nothing. And, doing fine. No extra pain, no major suffering. Like childbirth, I had managed to cut the cord and keep going.
Meeting with the Surgeon
So, nobody has asked the results of my surgery. You all assumed that because he says it went well right afterwards, that I'm fine now, isn't that true? You think he meant the cancer was cut out, and I am cured.
I wish.
I didn't speak to my surgeon for a couple of days after surgery. In fact, I only saw him twice the whole week (three times if you count the surgery date). He's clearly very important; it's obvious by the way everybody defers to him, and I only wish I could get people to treat me with that kind of respect and admiration. The only way it would happen for me at this point in my life is if I killed somebody in a spectacularly gruesome way and my celllies found out about it.
One thing you learn during a catastrophic illness such as stage IV metastatic breast cancer is the limits to medicine. And, there are so many. No matter how many imaging tests you have, something can be missed. You can have strange side effects that can't be diagnosed and even the best doctors can't figure it out.
You normal people tend to think that doctors know it all and the tests are perfect, and we who are very sick find that can be far from the truth, especially as things get more complicated. Diagnosing breast cancer? Easy. Diagnosing breathing problems after liver resection when angiograms and x-rays come out clean? Not so simple.
You normal people tend to think that doctors know it all and the tests are perfect, and we who are very sick find that can be far from the truth, especially as things get more complicated. Diagnosing breast cancer? Easy. Diagnosing breathing problems after liver resection when angiograms and x-rays come out clean? Not so simple.
The plan for me surgically was to cut me open (duh) then the SuperSurgeon was going to visually inspect my liver, looking for cancer any CT/PET scans had missed. (And, the fact that this is a routine part of surgery shows that missing cancer on CTs isn't.) Then he was going to use a sonogram - right on my actual liver - to see if there was anything there he couldn't see. Depending on what he or the sonogram saw, if there were any surprises, I may or may not have surgery or may have more ablation or less. If all was as expected, he would remove the left lobe of my liver and burn out the spot of cancer in the right lobe (using microwave ablation). If he saw something he wasn't expecting, he'd play it by ear.
Fortunately, his ears didn't need to be used. All my insides were as expected so he did the surgery as he expected. He told my husband all had gone well, meaning I'd survived the surgery, and he think he got it all, and that was it.
We rejoiced. I tweeted my cancer-free state.
They take your piece of liver off to pathology, of course, where it's dissected and inspected, and if you are Henrietta Lacks, used for many things. And, that's where things get a bit nerve-wracking for me. For my doctor came in a few days later and told me that the pathologist had found a spot of cancer on the removed section of liver that they had not seen visually, on CT, or even with the ultrasound right on the liver. "Fortunately, it's in the part we took out."
Although I would consider myself an optimist, his statement made me immediately wonder what was hiding in the part they didn't take out. Which, of course, I instantly said aloud. "If you found hidden cancer in the part you took out, doesn't that mean there could be some in the part you didn't?" He shrugged. He's also an optimist. He said, "The surgery went really well and the spot we found was really small and we got good margins." He can't know what he can't know.
None of us can, which is the lesson of cancer.
None of us can, which is the lesson of cancer.
I've been very eager to get back on chemo since that day, obviously. I hope that they got every spot of cancer, and that I will be cancer-free for the rest of my life, and I will be one of the miracle stories - one of the 2% who survive a diagnosis of metastatic cancer. It's what I desperately wanted to believe after this surgery. But there no assurances, and I knew that. Since he told me about the surprise cancer, I've never been able to "live the dream." In truth, I've been negative about it, or realistic, however you want to define it. I know what cancer is and does. Basically, at this point, it's a crapshoot as to whether I have cancer in my liver or not.
I have been working on being more positive in trying to believe they got it all out but that is not an easy thing to do when you are a realist. I even bought myself an encouraging bracelet, with three charms on it: Heal. Cure. Prevail. I look at it when I start to think time is still short for me, when I start to miss the grandchilden I've never had - to remind me that it's just as likely he did get it all and there is no surprise cancer. I have healed, I am cured, and I have prevailed.
I have been working on being more positive in trying to believe they got it all out but that is not an easy thing to do when you are a realist. I even bought myself an encouraging bracelet, with three charms on it: Heal. Cure. Prevail. I look at it when I start to think time is still short for me, when I start to miss the grandchilden I've never had - to remind me that it's just as likely he did get it all and there is no surprise cancer. I have healed, I am cured, and I have prevailed.
But insurance is good. I restarted chemo and herceptin on Friday, November 11, after 2 months absent. I was very ready. In three months, I'll have another PET/CT. That will hopefully show a clean liver as the ones I will do every three months from here on out will. At least, that is what I want to believe. Only time will tell.
And, finally, weaned off the epidural, eating hospital food ......I got to go home....
Don't forget to "like" me on facebook. I'm getting closer to my goal!
Don't forget to "like" me on facebook. I'm getting closer to my goal!
Thursday, November 10, 2011
I Left My Lobe in San Francisco: Liver Resection Hospitalization - Vignette 3&4
The Cancer Card
Liberal as San Francisco may be, there is still a shocking capitalistic side to it - all of the available rooms had quadrupled in rate.
UCSF has a recommended hotel section of its website, and most were listed in the very low $65.00 - $99.00 range which would be cheap, even for Sacramento. With rates like that, they really are doing hospital patients a favor.
But, not during Floricle.
Every place on that list I called was $400.00. Or more. A night. I expanded out from the recommendations, and all quotes were in the same range. And, I'm talking calling your crappy Motel 6 type places, not your luxury Top of the Mark hotels. At first, I'd just call and ask about rates. When I kept hearing $400.00, over and over, I realized I'd have to try a new tactic: playing the Cancer Card. So, I'd call and say, "Hello, my name is Ann, and I have breast cancer that has spread to the liver. I'll be staying at UCSF so they can take half my liver out and I need a place for my family to stay for the week - you were recommended by the hospital. Do you have a room?"
Hey, the hospital linked to them, they should have some empathy, right? A special rate (or a normal rate) for a patient?
The answer, despite my sob story, didn't change. It was either, "sorry, we are booked" or "yes, we have a room for $400.00 a night, would you like it? Even when I said, "But it says $70.00 on UCSF's website," I could hear the shrug over the phone. "It's Fleet Week and Oracle World, the entire city is booked."
Wait, I take it back, the story did change: some people added "I'm sorry, good luck to you," after they tried to get into my wallet. Most just hung up when I said I couldn't afford it.
I had two fall-backs. First, I knew the hospital had a social worker and thought she may have had some ideas. Second, my step-daughter just bought a house in South San Francisco. I knew that she'd be fine if we descended on her. I hesitated because I knew I would have to take up an entire bathroom the night before surgery, and I also wanted to be closer to the hospital. Plus, with my sister, my two sons and my son's girlfriend, it just seemed like too much of an imposition, especially staying for an entire week. She has a demanding job as a middle school teacher; she doesn't need people sleeping all over her house and hogging her bathroom.
But, it was in my back pocket in case I had to use it.
After dozens of phone calls, in despair, I shared my dilemma with a friend, who mentioned he'd stayed at the Cow Hollow Motor Inn and thought it was serviceable. I called them, and discovered - to my astonishment - they had not jacked up their rates and were even located in the heart of the city, on Lombard Street. I immediately booked it. Now, I am not going to say it was cheap - it wasn't. It was $130.00 a night, and that price didn't include luxury (it did include the smell of grease). But, it was clean and safe, and every staff member was extremely nice. The price gave me motive to get better so my husband could check-out, but it wasn't so high that I felt the need to leave the hospital and endanger myself.
The moral of the story is: sometimes, playing the cancer card doesn't work, even when the place you go to cure cancer recommends you play it.
(In fact, most of the time that card doesn't work, I really need to stop trying to pull it out.)
My Windows
As I said before, the view in my room was truly spectacular. There were a bank of windows, beginning in the bathroom (I didn't know that for a few days) stretching across to the other side. The entire City of San Francisco was displayed below like the sparkling jewel it is.
The photos I took didn't do it justice, not surprising considering they were taken by a woman cut wide open, sewn back together again, and lying flat on her back in a hospital bed. I tried to get my husband to take one, but every time he touches my iPhone, his hands shake - probably because he pays the bill. Trust me when I say that everybody who came in commented on the view - in most cases, before they commented on me. I'm surprised nobody brought it flowers. So many doctors walked in, never having seen the room before, and said, "Wow, look at that!" and they were not talking about my scar.
Which, by the way, is worth a comment or two. Or even flowers.
When you think about it, it's surprising that room is actually a hospital room. Although it's small, you'd think it would be the hospital boss's office, or a hideaway for his trysts, or a small conference room for heads of various departments. It could be rented it out for parties, or even become a small but very expensive San Francisco studio apartment - the view is that great. And, nobody would ever have to worry about getting sick living there. Because it had two sets of doors, it was extremely quiet - I heard no hospital noise at all. I have no doubt at all that my peaceful, pretty room contributed to my fast healing. Having privacy and a beautiful view - what more could you want?
Maybe some entertainment?
 |
| See the two spots sort of to the left? It's not dirt on your monitor - it's the Blue Angel's Aircraft |
Being a social sort, I invited everybody in for a party. "Hey, the Blue Angels will be practicing at 1:00, come back in," I'd tell the cleaning folks, the nursing staff, the doctors. I didn't have anything available to make it a real party - some leftover jello and a tea packet or two - and I wasn't sharing my dilaudid - but who cares? It was the Blue Angels! Several people did come by, stare out the window for a few minutes, then go about their business. They work hard at UCSF.
The real show was Saturday, the morning we were leaving, so practice was all we'd get to see. Their dry runs were so impressive, I can only imagine what the real thing looked like. After I checked out, I hope they managed to clean out my room and put another patient in there early enough so they could enjoy the spectacle.
It was very special to be able to see America's best and brightest share their talent in the skies during my recovery. As I saw the astounding tricks that must have taken tens of thousands of hours to learn, thinking about the dedication of those skilled pilots, I realized that inside the hospital the same kind of dedication was going on. The surgeon who took the chance and went against protocol to remove cancer from my liver, who spent decades honing his skill, who flew off in a different direction than the rest of his class by doing this surgery - what he did was every bit as beautiful as what the Blue Angels did.
I felt very lucky to be among the most skilled people in the world.
Happy Veteran's Day to all our remarkable service men and women.
Please help me meet my goal of getting 999 facebook likes. I don't know why I want to hit that number, but it feels lucky to me. So, if you have not liked his page yet, and you did like this post, please "like" me on facebook. I don't spam and you won't get a million status updates from me. You can do it to the right. Thanks!
Monday, November 7, 2011
I Left My Lobe in San Francisco: Liver Resection Hospitalization - Vignette 1&2
I was in the hospital for six days. Actually, I left the morning of the sixth day, and the first day I had surgery, so being an over-achiever, I am going to say recovery took me four days, with each day getting a bit easier on me.
One big help came when my sister took charge of one of the nurses. The majority of my experience with the nursing staff was outstanding, for which I am grateful after my last experience. This time, I was given appropriate care - with one exception.
First, let me explain: I have a theory about pain and pain medication which developed after my mastectomy/reconstruction, when I had to spend an extra day in the hospital due to poor pain management (and poor nursing care).I believe that pain control is key to recovery. The more relief you have, the more sleep you get, the more you can cooperate with the nurses when they ask you to get up, the more you can relax and let your body do the hard work of healing. When you are in pain, your muscles are tight, you can't sleep, your breathing is abnormal and it is much harder to recover. You don't get addicted to pain medicine during in the time you are in the hospital, at least not during a normal stay, so there is no reason at all not to take pain meds.
If you wanna be a tough guy, have at it. Me? I'm taking all they give me.
I discovered that is not only my theory. I was given brochures saying exactly this with my registration paperwork, and UCSF as a whole believes strongly in pain management. Still, traumatized by my experience at Mercy General, I mentioned pain control to all of my doctors, from SuperSurgeon, to Anesthesiologist, to Exhausted Med Student, and all agreed with me wholeheartedly, in both theory and prescribing.
The doctors prescribed IV pain meds, and told me I would transition to oral pain pills when I could eat, which would also signal to them that I was getting ready to go home. I was not expected to eat for a few days, which is normal after somebody has rearranged and removed part of your digestive system. I had an epidural with a button I could push for extra pain control every 15 minutes, and I was allowed a shot of dilaudid every two hours. They said I might be in pain a little between shots and they couldn't control it entirely, but would do the best they could and not to be afraid to call the nurses and get what I needed.
That sounded fair to me.
So, my one and only male nurse came in on Day One post-surgery. He introduced himself, and then stood at the foot of my bed and began his pain medicine lecture. He told me that he wanted me to take oral pain medicine since it would last longer in my body, and he would not be bringing me IV meds. I asked him what kind, and he said percocet.
As an aside, I know that percocet was not going to touch the pain that I had right then - 24 hours ago I'd been cut from between my breasts down to my waist, a major organ half removed and burned, and then sewed and stapled together. Percocet is what people take for headaches.
I was quite alarmed at his pronouncement. It was not a suggestion - he was telling me what he was going to do. He wasn't going to come in to give me shots. I knew I'd be under his care for at least 12 hours. I had flashbacks to my last hospitalization and became afraid.
I weakly argued with him, telling him that not only had I spoken to my doctors about what I should get - that very morning, in fact - and they wanted me on IV meds to be transitioned to oral when I could eat. I also told him my philosophy about pain relief, and I didn't believe a 5 mg percocet would give me relief for the kind of pain I was in - I'd taken it before and I knew. He didn't care about my thoughts, and stood there arguing with me. Literally arguing with a woman in my condition, despite my becoming visibly upset. Unfortunately, I didn't have breath or strength to become assertive about what I needed, which is where family comes in.
He left the room, and shortly after, my sister also left. I don't know what happened in that hallway except she spoke to the nurse. But I got my pain meds every two hours with no argument, and after that one day, he was not my nurse at all. For which I was extremely grateful.
I've come to believe he just didn't want to come in every two hours to give me pain relief. If he did think that oral pain meds were the better course for me, than he has missed his calling and should have gone to med school so he could prescribe what he wanted. My sister, after talking to him, also believes he just didn't want to be bothered every two hours.
The rest of the nurses gave me my ordered pain meds every time I asked for them, and each and every one of them were wonderful, even if I was annoying, which I'm sure every patient can be. I can't remember any of their names and I wish I'd written them down, because they deserve a paragraph about their kindness and understanding, rather than the one person who was only concerned about his own time.
I am especially grateful to the nurses aides (they have a fancy title that I forget). They were the ones who gave me a sponge bath, who helped me to the restroom, and who generally took care of all the icky things that have to be done. I dislike very much being dependent on anybody, and I'm sure I always will, but I'm grateful that these people were so kind.
Of course, once time, more than kindness brought them to my room..
I have a goal; I'm trying to get my facebook "likes" at 999. For no particular reason, other than everybody needs something to shoot for. So, if you have no liked his page yet, and you did like this post, please "like" me on facebook. You can do it to the right. Thanks!
After a day or two, I settled into a routine. I felt really good in the morning but at 3:30 I suddenly crumpled. The pain became intense, and I starting pushing the button for extra meds and watching the clock until I could get my next dose of dilaudid. I don't know why it happened in late afternoons, but it did. I was grateful (and surprised) to feel well for half the day though, and spent my time leafing through magazines, reading the paper, playing with my iPad and chatting with my family. I got out of bed and sat in the chairs for longer and longer periods each day. I had visits from my stepdaughter, which I much appreciated although she often came after work which was when the pain had hit and I was tired. It was nice for my husband though, who got to leave the hospital and take her for some food. Here's what I remember most about the hospital stay.
Hospital Vignettes
The Catheter
The Catheter
I was quite fearful the day they took the catheter out, which was the second day after surgery. The comfort of having a urinary bag cannot be over-estimated; I highly suggest you try it next time you feel like playing Farmville for three days straight. Style-wise? Well, they need some work. I'm not even sure Michael Kors could help with that, although wouldn't that be a fantastic challenge on Project Runway? "Make this catheter bag a style feature all women will want." Those runway models have a hard enough time walking in some of their shoes; let's add a catheter bag dangling down between their legs. Now, that's good TV!
Once I knew the catheter was coming out, and I'd have to get up to go like a normal person, the bathroom looked like it was 100 miles away: a trail littered with bones, rocks, sand, and the puddles of those who had come before me.
I knew I wouldn't make it.
The nursing staff put a commode near my bed, "just in case" and told me to call if I needed help. I was disgusted - me? A commode?
Peeing near your bed like a dog? No wait, even dogs don't pee near their beds. Peeing near your bed like some kind of wild animal, or hoarder who can't get through the newspaper pathways?
Not on your lfe.
I guess I don't value your life much.
It's the middle of the night. (Probably 9:30). I'm all alone and need to pee seriously bad. Why doesn't the CIA do this kind of torture? Hook somebody up to an IV that drips gallons of liquid into them, and then make it impossible to use the restroom? I'd tell state secrets, wouldn't you?
Anyway, I still had the epidural so my legs were numb and walking was impossible without help, plus unhooking an IV behind me on the wall was an issue - so the bathroom was out of the question unless I called an aide. That night, my nurse's aide was a man: a young, good-looking man. I'm still old-fashioned enough not to want a hot dude to help me take a pee.
That's for old ladies. Or fetishists.
There was nothing to do but use the commode. On my own. Without anybody to hold my hand. See, I told you I was a risk-taker.
I maneuvered myself like a snake to the side of the bed and used my bad arm to push myself up to a sitting position. It was one step to the commode but it was a complicated step - I had to put my hand on it to steady myself, pull my gown open in the back, move all the IV tubing, then pivot and sit, all with numb legs and a stapled stomach that could spill its contents at the smallest provocation.
But, I managed. I struggled, but I did it! Independence! I was sitting on a commode!
When you have an epidural, you can't really feel anything down there, or start or stop your flow properly - it just sort of.....happens. Numbly. So, I sat there for a while, hoping things would begin, imagining how it used to feel and hoping that would help, when I suddenly realized my wrinkled nude behind was facing the door, and the curtain covering the area only went to mid-back, and the light was shining under the curtain in my direction. Anybody who walked in (and in a hospital, everybody walks in) would be greeted by the site of my skinny rear, all lit up, spread out on a commode. And, given my condition, I would not be able to protect what was left of my dignity by covering myself.
Now, not only did I have to worry about how to start to pee, I had to worry about somebody coming in, seeing me in that compromising position, worry about protecting my personal privacy, and then getting a lecture on taking this huge risk and peeing alone.
Who could come in? What if it was a doctor wanting to discuss results? What if it was the cleaning man? What if it was a radiology tech? Do I sit and pee have a normal conversation like nothing was going on? Do I scream, "Get out!" Do I just pretend like I wanted to get up and that was the only place to sit, and nothing was happening?
Who could come in? What if it was a doctor wanting to discuss results? What if it was the cleaning man? What if it was a radiology tech? Do I sit and pee have a normal conversation like nothing was going on? Do I scream, "Get out!" Do I just pretend like I wanted to get up and that was the only place to sit, and nothing was happening?
I was trapped. I wanted to get this over with but while my mind was going a mile a minute, my hoo-haw was apparently in a coma.
Suddenly......ahh....relief. The stream started. I was peeing like a hoarder, right next to my bed. And peeing. And peeing some more. And urinating. And whizzing. And suddenly, I realized that that I possibly had a lot more pee in me than that container could hold.
But I couldn't stop, my bladder was open and there was no way to shut it.
Add overflow to my list of worries.
Add overflow to my list of worries.
Fortunately, I finished right in time. The urine level was so high up that the person who later had to dump it not only commented but had to be very careful taking it to the toilet. "Wow, you must have really had to go."
Hospital personnel are masters of understatement.
Hospital personnel are masters of understatement.
Anyway, after I was done, feeling quite successful (and proud that I'd remembered to grab a tissue), I gathered myself, weakly got back up, and somehow got back into bed. And slept, quite well, right next to a full bucket of pee.
 |
| No, this isn't me, but doesn't she look happy? |
Pain Control
The first day post-surgery was a blur of pain. Again, I have to mention how grateful I am to my family, who helped in so many ways, big and small; from handing me things I couldn't get on my own, to talking to medical professionals, to keeping me company. I highly recommend that if you have an upcoming hospital stay, you find one person willing to spend time with you, even if you have to pay them. It makes things so much easier.
One big help came when my sister took charge of one of the nurses. The majority of my experience with the nursing staff was outstanding, for which I am grateful after my last experience. This time, I was given appropriate care - with one exception.
First, let me explain: I have a theory about pain and pain medication which developed after my mastectomy/reconstruction, when I had to spend an extra day in the hospital due to poor pain management (and poor nursing care).I believe that pain control is key to recovery. The more relief you have, the more sleep you get, the more you can cooperate with the nurses when they ask you to get up, the more you can relax and let your body do the hard work of healing. When you are in pain, your muscles are tight, you can't sleep, your breathing is abnormal and it is much harder to recover. You don't get addicted to pain medicine during in the time you are in the hospital, at least not during a normal stay, so there is no reason at all not to take pain meds.
If you wanna be a tough guy, have at it. Me? I'm taking all they give me.
I discovered that is not only my theory. I was given brochures saying exactly this with my registration paperwork, and UCSF as a whole believes strongly in pain management. Still, traumatized by my experience at Mercy General, I mentioned pain control to all of my doctors, from SuperSurgeon, to Anesthesiologist, to Exhausted Med Student, and all agreed with me wholeheartedly, in both theory and prescribing.
The doctors prescribed IV pain meds, and told me I would transition to oral pain pills when I could eat, which would also signal to them that I was getting ready to go home. I was not expected to eat for a few days, which is normal after somebody has rearranged and removed part of your digestive system. I had an epidural with a button I could push for extra pain control every 15 minutes, and I was allowed a shot of dilaudid every two hours. They said I might be in pain a little between shots and they couldn't control it entirely, but would do the best they could and not to be afraid to call the nurses and get what I needed.
That sounded fair to me.
So, my one and only male nurse came in on Day One post-surgery. He introduced himself, and then stood at the foot of my bed and began his pain medicine lecture. He told me that he wanted me to take oral pain medicine since it would last longer in my body, and he would not be bringing me IV meds. I asked him what kind, and he said percocet.
As an aside, I know that percocet was not going to touch the pain that I had right then - 24 hours ago I'd been cut from between my breasts down to my waist, a major organ half removed and burned, and then sewed and stapled together. Percocet is what people take for headaches.
I was quite alarmed at his pronouncement. It was not a suggestion - he was telling me what he was going to do. He wasn't going to come in to give me shots. I knew I'd be under his care for at least 12 hours. I had flashbacks to my last hospitalization and became afraid.
I weakly argued with him, telling him that not only had I spoken to my doctors about what I should get - that very morning, in fact - and they wanted me on IV meds to be transitioned to oral when I could eat. I also told him my philosophy about pain relief, and I didn't believe a 5 mg percocet would give me relief for the kind of pain I was in - I'd taken it before and I knew. He didn't care about my thoughts, and stood there arguing with me. Literally arguing with a woman in my condition, despite my becoming visibly upset. Unfortunately, I didn't have breath or strength to become assertive about what I needed, which is where family comes in.
He left the room, and shortly after, my sister also left. I don't know what happened in that hallway except she spoke to the nurse. But I got my pain meds every two hours with no argument, and after that one day, he was not my nurse at all. For which I was extremely grateful.
I've come to believe he just didn't want to come in every two hours to give me pain relief. If he did think that oral pain meds were the better course for me, than he has missed his calling and should have gone to med school so he could prescribe what he wanted. My sister, after talking to him, also believes he just didn't want to be bothered every two hours.
The rest of the nurses gave me my ordered pain meds every time I asked for them, and each and every one of them were wonderful, even if I was annoying, which I'm sure every patient can be. I can't remember any of their names and I wish I'd written them down, because they deserve a paragraph about their kindness and understanding, rather than the one person who was only concerned about his own time.
I am especially grateful to the nurses aides (they have a fancy title that I forget). They were the ones who gave me a sponge bath, who helped me to the restroom, and who generally took care of all the icky things that have to be done. I dislike very much being dependent on anybody, and I'm sure I always will, but I'm grateful that these people were so kind.
Of course, once time, more than kindness brought them to my room..
I have a goal; I'm trying to get my facebook "likes" at 999. For no particular reason, other than everybody needs something to shoot for. So, if you have no liked his page yet, and you did like this post, please "like" me on facebook. You can do it to the right. Thanks!
Sunday, November 6, 2011
I Left My Lobe in San Francisco: Liver Resection Story. Family
I know it's been a while since I wrote. I recovered, and started puttering around the house- too busy to post. Then I had a set-back and it now is very hard to write. But, I'm going to ignore my discomfort as I know many of you are getting freaked. And, being the a-z creature I am, I'll continue where I left off
Back on Mickey's Hospital Land Ride, I was pushed down a corridor, where I groggily passed a pretty woman. She said "hi" to me and I said "hi" back. Her hair was up and I thought she was a nurse who was going to help take me to my room - then suddenly I realized that beautiful woman was my sister! I smiled big and said, "Oh hi!"
I think for a second she thought I'd had a stroke or something for not recognizing her.
I was right though, she was going with me to my room, as was the rest of my family; my husband and my two boys - they all surrounded my bed like little satellites.
What would life be like without family to help you through your worst moments?
As hard as the day had been for me, I knew it had been harder for my family. I'd slept through most of it, and I was getting dialudid to help me cope with being awake. They were not so lucky.
They had spent most of the day in a hospital waiting room, with no news about my condition. Even when they got news that I was okay it was many more hours before they could see me.
Everybody had taken time off work and school - my sister had come 600 miles for what she knew in advance would be a bad experience, even a nightmarish one. We had to take my son out of school, and he's one of those super-star students who is tortured by missing school. (When I was in high school I'd have gladly had everybody in my family have surgery if I could miss one day, and in fact, contemplated making that happen.)
I was comforted knowing they were there, and it's not lost on me that they put aside their discomfort to be there for me. I can only imagine what they went through during the 12 hours I was unavailable to them.
Collectively, me on a gurney and them surrounding me, we went through a set of double-doors into an air-lock type area with a laundry bin, and then through another set of double-doors to my room. As we walked through, the nurse told me my room was on the 13th floor and I was in Room 1331, and said, "I hope you aren't superstitious."
Nope. You could name my room, 666 Malpractice Death Wing, and I'd be fine as long as it was a private room.
It was dark, and all I saw were a bank of windows, black as night. The nurse told me that you could see the lights of the city, but without my contacts, I wasn't impressed. I was impressed by the fact that there was only one bed in that room.
That first night is pretty fuzzy. I don't remember how long my family stayed or much of anything that happened. I know my sister spent the night with me one night, but not the first. The large doses of painkillers I was getting, combined with recent anesthesia created a dream-like situation. I think my exhausted family left as soon as they saw I was settled in. I do remember at one point in the middle of the night nurses and rads techs came to take a chest x-ray and that hurt as they had to roll me on my side to get the board under me. I don't recall asking for pain meds - but I'm sure I did I don't recall pushing the button on my epidural for extra doses - but I'm sure I did. It was probably a bad night but I honestly don't remember now.
Morning dawned, and I realized I not only had a private room, I had one with an incredible view. I was now not only happy with the room, I was bragging!
I had a sweeping, panoramic view of San Francisco, from the TransAmerica Building all the way to the Golden Gate Bridge. It was spectacular, and all mine. I grabbed my iphone and ignored the extreme and searing pain to tweet that view, and shame on you who aren't following me @butdocihatepink
Unbelievably, the day after my surgery -the surgery where I was flayed from mid-chestbone to belly button and across to my waist - AND had half my liver removed and burned - the sadistic nurses wanted me standing up. On my feet! With a catheter bag dangling down. Well, I don't have to tell you that was quite painful, and they didn't want me to just stand, they wanted me to move my legs back and forth. I lost my footing and sat down back to bed, suddenly (ouch) but got up to try again because I'm super brave and all that BS. (The sooner you do it, the sooner they leave). The second time I managed to do the Hustle as requested, then I got a sponge bath and went back to bed.
I felt better after getting up, hard as it was. If you have found this blog because you are having a liver resection, don't resist standing up. It jump starts your recovery.
They also gave me an inspiration spirometer to practice breathing - it helps prevent pneumonia. I was to practice it once an hour and get the little ball to a line she drew. I'm pretty sure I didn't do it once an hour - it wasn't that inspiring - but I did it several times a day. I never did meet my goal, however.
I'm not sure I could meet it now, but that's a different story.
Back on Mickey's Hospital Land Ride, I was pushed down a corridor, where I groggily passed a pretty woman. She said "hi" to me and I said "hi" back. Her hair was up and I thought she was a nurse who was going to help take me to my room - then suddenly I realized that beautiful woman was my sister! I smiled big and said, "Oh hi!"
I think for a second she thought I'd had a stroke or something for not recognizing her.
I was right though, she was going with me to my room, as was the rest of my family; my husband and my two boys - they all surrounded my bed like little satellites.
What would life be like without family to help you through your worst moments?
As hard as the day had been for me, I knew it had been harder for my family. I'd slept through most of it, and I was getting dialudid to help me cope with being awake. They were not so lucky.
They had spent most of the day in a hospital waiting room, with no news about my condition. Even when they got news that I was okay it was many more hours before they could see me.
Everybody had taken time off work and school - my sister had come 600 miles for what she knew in advance would be a bad experience, even a nightmarish one. We had to take my son out of school, and he's one of those super-star students who is tortured by missing school. (When I was in high school I'd have gladly had everybody in my family have surgery if I could miss one day, and in fact, contemplated making that happen.)
I was comforted knowing they were there, and it's not lost on me that they put aside their discomfort to be there for me. I can only imagine what they went through during the 12 hours I was unavailable to them.
Collectively, me on a gurney and them surrounding me, we went through a set of double-doors into an air-lock type area with a laundry bin, and then through another set of double-doors to my room. As we walked through, the nurse told me my room was on the 13th floor and I was in Room 1331, and said, "I hope you aren't superstitious."
Nope. You could name my room, 666 Malpractice Death Wing, and I'd be fine as long as it was a private room.
It was dark, and all I saw were a bank of windows, black as night. The nurse told me that you could see the lights of the city, but without my contacts, I wasn't impressed. I was impressed by the fact that there was only one bed in that room.
That first night is pretty fuzzy. I don't remember how long my family stayed or much of anything that happened. I know my sister spent the night with me one night, but not the first. The large doses of painkillers I was getting, combined with recent anesthesia created a dream-like situation. I think my exhausted family left as soon as they saw I was settled in. I do remember at one point in the middle of the night nurses and rads techs came to take a chest x-ray and that hurt as they had to roll me on my side to get the board under me. I don't recall asking for pain meds - but I'm sure I did I don't recall pushing the button on my epidural for extra doses - but I'm sure I did. It was probably a bad night but I honestly don't remember now.
Morning dawned, and I realized I not only had a private room, I had one with an incredible view. I was now not only happy with the room, I was bragging!
I had a sweeping, panoramic view of San Francisco, from the TransAmerica Building all the way to the Golden Gate Bridge. It was spectacular, and all mine. I grabbed my iphone and ignored the extreme and searing pain to tweet that view, and shame on you who aren't following me @butdocihatepink
Unbelievably, the day after my surgery -the surgery where I was flayed from mid-chestbone to belly button and across to my waist - AND had half my liver removed and burned - the sadistic nurses wanted me standing up. On my feet! With a catheter bag dangling down. Well, I don't have to tell you that was quite painful, and they didn't want me to just stand, they wanted me to move my legs back and forth. I lost my footing and sat down back to bed, suddenly (ouch) but got up to try again because I'm super brave and all that BS. (The sooner you do it, the sooner they leave). The second time I managed to do the Hustle as requested, then I got a sponge bath and went back to bed.
I felt better after getting up, hard as it was. If you have found this blog because you are having a liver resection, don't resist standing up. It jump starts your recovery.
They also gave me an inspiration spirometer to practice breathing - it helps prevent pneumonia. I was to practice it once an hour and get the little ball to a line she drew. I'm pretty sure I didn't do it once an hour - it wasn't that inspiring - but I did it several times a day. I never did meet my goal, however.
I'm not sure I could meet it now, but that's a different story.
Tuesday, October 25, 2011
Quick Note
I have a blog post about my hospitalization half written, and then I realized I needed a nap.
And, that nap hasn't really ended yet. I'm resting, healing, and doing nothing. I'm fine but don't have a lot of energy so am piddling around these days. What is sucky about being home like this is all those projects you wanted to start - you don't have the energy. As soon as I go back to work, then I'll be mad I didn't start the projects.
Anyway, I'll try to finish that post soon, as I want anybody who has even the smallest possibility of getting this surgery to know what it's like.
But, one thing it's like is being tired.
See ya soon!
And, that nap hasn't really ended yet. I'm resting, healing, and doing nothing. I'm fine but don't have a lot of energy so am piddling around these days. What is sucky about being home like this is all those projects you wanted to start - you don't have the energy. As soon as I go back to work, then I'll be mad I didn't start the projects.
Anyway, I'll try to finish that post soon, as I want anybody who has even the smallest possibility of getting this surgery to know what it's like.
But, one thing it's like is being tired.
See ya soon!
Wednesday, October 12, 2011
I Left My Lobe in San Francisco: Liver Resection Story. Surgery
I went feet first through double-doors which automatically opened and closed behind me, like a Disneyland B-Ticket Ride; "Mickey's Hospital World." My gurney rumbled down a hallway, one decorated the length of the corridor with dozens of white coats hanging from knobs. It reminded me of Hell's Kitchen with all the chef's coats skewered on meat hooks and flames wiping away the picture of the cook who'd been eliminated. We flew past Disney's Hall of Coats and then on the left hand side we encountered a line of physicians behind glass scrubbing for their upcoming surgeries. I went through another set of wacky double-doors, and there I was - in the operating room.
And, I have to say, it looked exactly like the operating rooms you see on TV. Everything was gleaming and expansive. Overhead were shining mirrored lights, cabinets glowing with drugs, instruments sparkling on tables, doctors gloved and ready.....
...okay, no it didn't.
It looked like my office storage room, before I make my TAs clean it each year.
Over to the right was my surgeon standing behind a jumbled pile of boxes near a whiteboard, talking to another doctor. There was an x-ray on the lightbox which I thought could be mine but then I saw somebody else's name on it. There were nurses moving around, again behind what appeared to be open boxes, maybe from Amazon or the Home Shopping Network. There was stuff piled in corners, and the shelves were haphazard - it looked pretty ordinary, and kind of like they put an operating room in the middle of a cellar.
The Anesthesiologist explained that they were going to put the epidural in first, and alarmed me by saying this was one of the most painful surgeries they do but the epidural would help. He asked me to sit up and bend forward over the gurney railing, which I did. As all pregnant women know, an epidural is a small tube inserted directly into your spinal canal that drips medicine in to give you pain relief. As they struggled to get the tube in the right place, I became frustrated, because I could hear my surgeon talking about my very own personal operation with his colleague, and it sounded like he was discussing odds and new theory and what was best and giving a lesson on ablation, and I really wanted to hear that. But, the tube wasn't going in properly and the anesthesiology team kept talking to me, each other, and everyone else, so I couldn't hear my surgeon's very interesting conversation.
Tube finally in my spine, they moved me from the gurney to the operating table. They were serious when they said they hoped I had the temperpedic one. (I didn't). I didn't think I'd care very much although I thought a temperpedic operating table an interesting idea. I reminded them about my frozen shoulder, and they said my arm would be down by my side and not to worry. They gave me a hat to put on and then said they would give me medicine to put me to sleep now. They put a mask over my face and I breathed in the plastic scent for quite a while, looking around, blinking now and then.
Nothing.
I began to wonder if I was going to go to sleep, or if, like Michael Jackson, I was immune and was going to have to grab the bottle of propofol and take a slug myself. Had they asked me to count down from 10 (for you surgery newbies, they never do), I would have done so easily - and than then what?
We'll never know because I'm no Jackson, and I did go out.
And, ladies and gentlemen, had I not survived the surgery, those would have been my last thoughts on this earth: Michael Jackson, Propofol, and WTF - when am I going out?
Not exactly profound.
I woke up to chaos. It's pretty fuzzy, but I was in the same place I'd been in the morning, which is PACU (Post-Anesthesia Care Unit). It was about 1:30 and I was told I was fine and the operation had gone well. This was the first time they asked me that pain scale question I hate so much, but when your pain is a 10 it's not so hard to answer.
I was in terrible pain, and I know I drifted in and out as they tried to get a handle on it. I don't remember everything they did but they kept shooting me up with drugs, and I don't think my epidural was working, or it wasn't turned on, for quite a while, or maybe that's my imagination.
I have to say that the nurses in that area were quite kind. I shared a nurse with one other person, and she took good care of me. I was unable to move, really think or do much but suffer for the longest time.
Eventually, they got a handle on it and asked me if I wanted my husband. I said I did, but she forgot to call him and I didn't have the knowledge of time passing to remind her. I think this happened a few times until she finally remembered, and by then it was about 7:30. That's a long time to make family wait. I realized they they didn't want my family to see me until the pain was under control, but she shouldn't have forgotten. My sister finally called up and said they wanted to see me now, and that's when the nurse remembered and allowed him to come see me.
As I recovered I also got to see the rest of my family, which was nice, and which I'm sure helped. I was happy to be alive, although considering the pain, not ecstatic. I found out from my husband that the surgeon was very happy with the results he got. He'd told my husband that they had taken all of the left lobe of the liver. They couldn't take the cancerous part of the right lobe because it was too deep and would have been dangerous, but that the remaining tumor was extremely small so they used the microwave ablation tool to burn it off with a 2 inch margin, and he was extremely pleased and felt things had gone as well as possible.
I realized, despite the pain, that I was now cancer-free.
I don't have cancer.
I eventually found out I had to stay in PACU until I told them my pain was down to a five, so the next time they asked, that's what I told them. I was ready to get out of there, I was the only patient who'd been there that long.
That pain scale is all subjective anyway; hell, maybe it was even was a five.
Now that they'd decided to move me to a room the nurse got on the phone with the reservation desk and turned to me and asked me if I'd requested a private room. I said I'd had. Indeed, I'd called a week ago and made that request. I'd been told repeatedly that it was unlikely I'd get one, so I was extremely happy to find that I was, indeed, assigned a private room.
Even in my pain and drug-fueled fog, I was thrilled at that. Nobody else's farts, foul smells, complaints, groans, visitors or endless TV would interfere with my own suffering and healing. I would get to be alone, except for my family.
I couldn't have been happier.
Until I saw the room.....
And, I have to say, it looked exactly like the operating rooms you see on TV. Everything was gleaming and expansive. Overhead were shining mirrored lights, cabinets glowing with drugs, instruments sparkling on tables, doctors gloved and ready.....
...okay, no it didn't.
It looked like my office storage room, before I make my TAs clean it each year.
Over to the right was my surgeon standing behind a jumbled pile of boxes near a whiteboard, talking to another doctor. There was an x-ray on the lightbox which I thought could be mine but then I saw somebody else's name on it. There were nurses moving around, again behind what appeared to be open boxes, maybe from Amazon or the Home Shopping Network. There was stuff piled in corners, and the shelves were haphazard - it looked pretty ordinary, and kind of like they put an operating room in the middle of a cellar.
The Anesthesiologist explained that they were going to put the epidural in first, and alarmed me by saying this was one of the most painful surgeries they do but the epidural would help. He asked me to sit up and bend forward over the gurney railing, which I did. As all pregnant women know, an epidural is a small tube inserted directly into your spinal canal that drips medicine in to give you pain relief. As they struggled to get the tube in the right place, I became frustrated, because I could hear my surgeon talking about my very own personal operation with his colleague, and it sounded like he was discussing odds and new theory and what was best and giving a lesson on ablation, and I really wanted to hear that. But, the tube wasn't going in properly and the anesthesiology team kept talking to me, each other, and everyone else, so I couldn't hear my surgeon's very interesting conversation.
Tube finally in my spine, they moved me from the gurney to the operating table. They were serious when they said they hoped I had the temperpedic one. (I didn't). I didn't think I'd care very much although I thought a temperpedic operating table an interesting idea. I reminded them about my frozen shoulder, and they said my arm would be down by my side and not to worry. They gave me a hat to put on and then said they would give me medicine to put me to sleep now. They put a mask over my face and I breathed in the plastic scent for quite a while, looking around, blinking now and then.
Nothing.
I began to wonder if I was going to go to sleep, or if, like Michael Jackson, I was immune and was going to have to grab the bottle of propofol and take a slug myself. Had they asked me to count down from 10 (for you surgery newbies, they never do), I would have done so easily - and than then what?
We'll never know because I'm no Jackson, and I did go out.
And, ladies and gentlemen, had I not survived the surgery, those would have been my last thoughts on this earth: Michael Jackson, Propofol, and WTF - when am I going out?
Not exactly profound.
 |
| Then they did the operation |
I woke up to chaos. It's pretty fuzzy, but I was in the same place I'd been in the morning, which is PACU (Post-Anesthesia Care Unit). It was about 1:30 and I was told I was fine and the operation had gone well. This was the first time they asked me that pain scale question I hate so much, but when your pain is a 10 it's not so hard to answer.
I was in terrible pain, and I know I drifted in and out as they tried to get a handle on it. I don't remember everything they did but they kept shooting me up with drugs, and I don't think my epidural was working, or it wasn't turned on, for quite a while, or maybe that's my imagination.
I have to say that the nurses in that area were quite kind. I shared a nurse with one other person, and she took good care of me. I was unable to move, really think or do much but suffer for the longest time.
Eventually, they got a handle on it and asked me if I wanted my husband. I said I did, but she forgot to call him and I didn't have the knowledge of time passing to remind her. I think this happened a few times until she finally remembered, and by then it was about 7:30. That's a long time to make family wait. I realized they they didn't want my family to see me until the pain was under control, but she shouldn't have forgotten. My sister finally called up and said they wanted to see me now, and that's when the nurse remembered and allowed him to come see me.
As I recovered I also got to see the rest of my family, which was nice, and which I'm sure helped. I was happy to be alive, although considering the pain, not ecstatic. I found out from my husband that the surgeon was very happy with the results he got. He'd told my husband that they had taken all of the left lobe of the liver. They couldn't take the cancerous part of the right lobe because it was too deep and would have been dangerous, but that the remaining tumor was extremely small so they used the microwave ablation tool to burn it off with a 2 inch margin, and he was extremely pleased and felt things had gone as well as possible.
I realized, despite the pain, that I was now cancer-free.
I don't have cancer.
I eventually found out I had to stay in PACU until I told them my pain was down to a five, so the next time they asked, that's what I told them. I was ready to get out of there, I was the only patient who'd been there that long.
That pain scale is all subjective anyway; hell, maybe it was even was a five.
Now that they'd decided to move me to a room the nurse got on the phone with the reservation desk and turned to me and asked me if I'd requested a private room. I said I'd had. Indeed, I'd called a week ago and made that request. I'd been told repeatedly that it was unlikely I'd get one, so I was extremely happy to find that I was, indeed, assigned a private room.
Even in my pain and drug-fueled fog, I was thrilled at that. Nobody else's farts, foul smells, complaints, groans, visitors or endless TV would interfere with my own suffering and healing. I would get to be alone, except for my family.
I couldn't have been happier.
Until I saw the room.....



